We have read with great interest the exogenous lipoid pneumonia (ELP) case series from Latorre et al.,1 which elegantly demonstrates the radiological findings inherent to pathological aspiration of petroleum jelly (Vaseline). The authors report that the most common high-resolution computed tomography (HRCT) findings in ELP are areas of low attenuation and ground glass opacity (GGO). However, on careful analysis, the CT images for Case 1 exclusively show peribronchial consolidation tissue, but no areas of GGO. The second case reported, supported by CT, CT-PET and MRI, very clearly shows fat in middle lobe. Some of the clinical cases did not have an accompanying radiological image. We respectfully would like to share our experience of two cases of aspiration of oily product, used for cleaning the stoma in adult patients (a 63-year-old woman and a 68-year-old man) after laryngectomy for cancer. Our patients showed an extended GGO component in the middle lobe, lingula and lower lobes, confirmed on bronchoalveolar lavage testing to be alveolar lipid-laden macrophages. Despite the administration of corticosteroids for a period of 6 months (after discontinuing the use of Vaseline), the results were very disappointing: the man showed absolute stability of the HRCT findings and the woman's GGO component continued to worsen, to a greater extent in the lower lobes (Fig. 1). The clinical conditions of both patients worsened with further marked reduction in DLCO in both cases. We are aware that this deterioration could be associated with an increased of level of inflammation due to fatty acids, as described in a recent paper.2 Fatty acids either remain in the alveolar compartment or are phagocytized by macrophages that then migrate to the interlobular septa. This phenomenon could partly explain the meaning of the “crazy paving” pattern observed on HRCT.3 However, we assume that reactivity of the affected lung is also consistent with organizing pneumonia, leading to toxic lung injury.4 Due to their critical clinical status, our patients could not undergo a lung biopsy so our findings unfortunately remain only a hypothesis. To sum up, HRCT is the best imaging modality for establishing the diagnosis of lipoid pneumonia. However, there is an important issue which needs clarification: according to Marchiori et al.,5 consolidation is common in children, while GGO and crazy paving are more often seen in adults. The question here is why, after treatment, do areas of GGO and crazy paving sometimes become more extended but with no signs of fibrosis. In conclusion, in patients with pathological findings due to aspiration of petroleum jelly used to clean the tracheostoma, a careful clinical evaluation with FEV1 spirometry and possibly low dose HRCT with narrowed slices is recommended in cases in which GGO is a dominant HRCT pattern.
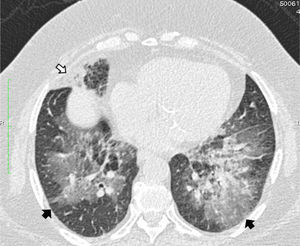
High resolution computed tomography scan of the chest shows peribronchial fat consolidation in middle lobe (white arrows). Extensive representation of GGO containing subtle reticulation (crazy paving) up to pleural spaces (black arrows) 8 months after discontinuing petroleum jelly (Vaseline) and steroid therapy (prolonged for 6 months).
Please cite this article as: Rea G, Lassandro F, Valente T. Neumonía lipoidea exógena en pacientes laringectomizados: ¿es el patrón de opacificación en vidrio esmerilado/en empedrado una reacción organizada de la neumonía capaz de predecir una mala evolución?. Arch Bronconeumol. 2016;52:438–439.