The incidence of bronchiectasis is increasing, especially among older patients.1 Bronchiectasis occurs with exacerbations, which, when coupled with respiratory failure, hemodynamic instability, sepsis, or other complications, may require a hospital stay.2 These hospitalizations generate a heavy economic burden,3,4 which increases with severity and readmissions.4 Our objective was to analyze trends in admissions for bronchiectasis exacerbations over a period of 10 years.
The study included all discharges coded 494.1 (bronchiectasis exacerbation) according to the International Code of Diseases version 9 (ICD-9) as primary diagnosis, between the years 2008 and 2017, in the Hospital Universitario Germans Trias i Pujol. The linear trend and trend in proportions were analyzed using the nptrend and ptrend commands in Stata® version 15, respectively. The study was approved by the Ethics Committee of the Hospital Universitari Germans Trias i Pujol.
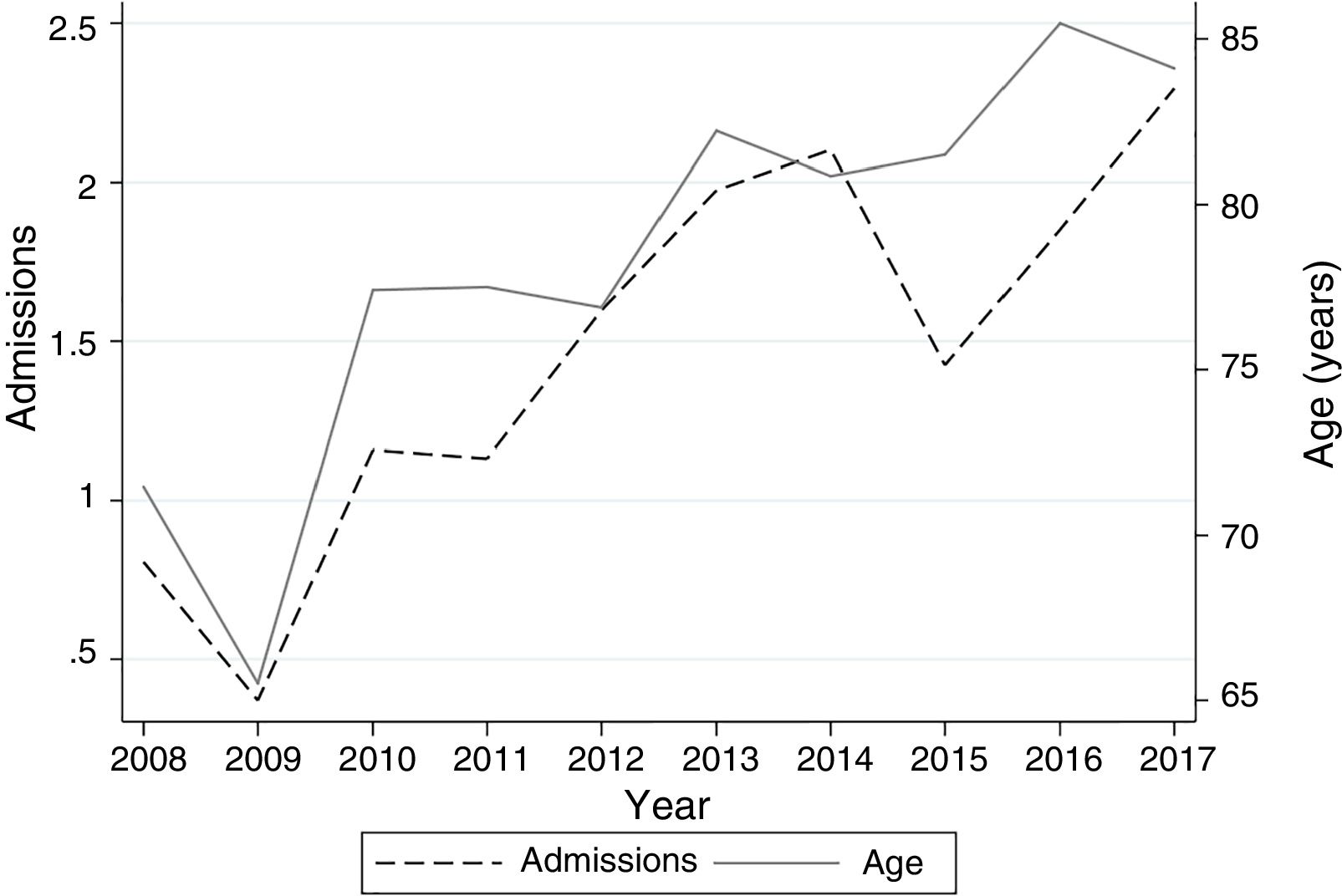
During the study period, there were 304 admissions with bronchiectasis exacerbation as a primary diagnosis, in a total of 190 patients. Of these, 136 patients (71.6%) had 1 admission, 36 (18.9%) 2 admissions, 6 (3.2%) 3 admissions, and 6.3% 4 or more admissions. Of these, 75.1% were women with a mean age of 80.3 years (SD: 6.1). Mean stay was 9.5 (SD: 2.0). In-hospital mortality rate was 3.7%, with a 30-day readmission rate of 11.7%. Mortality was not significantly associated with age (P=.08) nor with the number of admissions (P=.11). The proportion of admissions with bronchiectasis as primary diagnosis compared to total admissions in our hospital was 2.29 per 1000. No significant changes occurred in readmission rates, mortality, and length of stay over the period analyzed. On the other hand, a significant increase was observed in the age of patients (P<.01) and in the proportion of admissions for bronchiectasis compared to the total number of admissions in our hospital (P<.01) (Fig. 1).
shows the progress of numbers of admissions for bronchiectasis and age over the study period. The left y-axis displays the number of admissions/1000 for bronchiectasis compared to total admissions during the time period analyzed. The right y-axis shows the average age of patients in years.
Although some authors have described falling admission rates for acute exacerbations of bronchiectasis,5 most of the existing studies coincide with ours, and report increasing rates of admissions for this reason.6,7 Sanchez-Munoz et al.,8 unlike us, described a decline in admissions when bronchiectasis exacerbation was the primary diagnosis, but when it was a secondary diagnosis, admissions increased. We did not include admissions for bronchiectasis exacerbation as a secondary diagnosis in our study.
With regard to the length of hospital stay of these patients, other authors in general describe a reduction in length of stay,8,9 which is around 11 days.7,8 Similarly to other reports,9 when readmissions were analyzed, no changes were observed over the study period. As for mortality, we did not find significant variations over time, unlike other previously published studies that describe a decrease.9 Again, Sanchez-Munoz et al. found differences depending on whether the diagnosis was the principal or secondary diagnosis.8
Our study has clear limitations. It is retrospective, so we were unable to analyze the criteria for admission of patients, associated co-morbidities, and antibiotic treatment (type, duration, etc.) received, factors that clearly have a role in patient prognosis. It is also possible that the increasing number of diagnoses is due not to a real higher incidence, but rather to a greater awareness of the disease and better coding in the hospital.
In summary, we found an increase in the number of admissions for bronchiectasis, and in the age of patients over the time period analyzed. There were no changes in mortality, readmission rates, or length of stay. It would be interesting to perform a multicenter study to analyze in more detail the factors associated with the prognosis of patients admitted for bronchiectasis exacerbations.
Please cite this article as: Garcia-Olivé I, Marin A, Rodríguez-Pons L, Abad J. Evolución de los ingresos por bronquiectasias en un hospital de tercer nivel (2008-2017). Arch Bronconeumol. 2019;55:217–218.