Airway complications after lung transplant are relatively common although the rates vary according to the different studies. Pathogenesis is diverse but the principal mechanism is usually bronchus intermedius ischemia in the post-transplant period. One major complication is bronchial stenosis, with relatively frequent involvement of the bronchus intermedius in the case of right lung transplantation. Various treatments have been proposed for bronchus intermedius stenosis, such as endobronchial balloon dilation, laser, cryosurgery and bronchial stents. We present two cases of lung transplant recipients with bronchus intermedius stenosis treated with a Montgomery stent or T-stent, commonly used for tracheal stenosis, who showed positive clinical and functional response.
Las complicaciones de la vía aérea en pacientes con trasplante pulmonar son una entidad relativamente frecuente, aunque su incidencia es variable según los diferentes estudios. Su patogenia es variada, siendo el principal mecanismo responsable la isquemia bronquial asociada al periodo postrasplante inmediato. La principal complicación suele ser la estenosis bronquial, y en el trasplante pulmonar derecho la afectación del bronquio intermediario se produce con relativa frecuencia. Se han propuesto distintos tratamientos para la estenosis del bronquio intermediario, como dilatación con balón endobronquial, láser, criocirugía y endoprótesis bronquiales. Presentamos 2 casos clínicos con trasplante pulmonar y estenosis del bronquio intermediario que han sido tratados con una endoprótesis de Montgomery o en T, que se emplea habitualmente para estenosis traqueales, con una respuesta clínica y funcional muy favorable.
Airway complications after lung transplantation (LT) remain a significant source of morbidity and mortality, despite improvements in surgical techniques and immunosuppressive treatment.
An incidence of between 7% and 18% is reported, mainly because there is no standard definition of these complications and a universally accepted classification system has not yet been defined. Associated mortality ranges from 2% to 4%.1
Several endoscopic techniques are employed in the treatment of bronchus intermedius (BI) stenosis, such as endobronchial balloon dilation, laser, cryosurgery and bronchial stents. The main disadvantages of endobronchial stent placement are the risk of obstructing the right upper lobe (RUL) orifice2 and the development of restenosis in the upper section of the stent, suggesting that the Montgomery stent may be a new solution.
Clinical ObservationClinical Case 1A 62-year-old man who underwent right unilateral LT in June 2011.
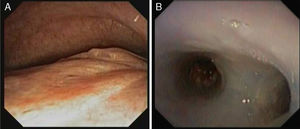
The patient's initial clinical progress was good, but 4 months after the intervention he was hospitalized for respiratory failure due to Pseudomonas aeruginosa superinfection. Fiberoptic bronchoscopy (FB) was performed, revealing significant BI stenosis with evidence of malacia distal to the right main bronchial anastomosis (Fig. 1A). Bronchial lumen on expiration was reduced to 25%.
Our initial decision was to place an AERO self-expanding bronchial stent in the BI using rigid bronchoscopy. After the procedure, the patient had some repeated obstructive episodes due to secretions, so the AERO stent was replaced with a Dumon silicone stent. However, the episodes did not resolve.
Three months later (13 months post-transplantation), the Dumon stent was removed and replaced with a Montgomery stent that had previously been cut according to the measurements of airway to be treated, determined on endoscopic examination (outer diameter 12mm, total length 4.5cm, length of proximal limb 1.5cm, length of distal limb 1.5cm). The horizontal limb of the device was placed in the RUL, the proximal part in the mid-section of the right main bronchus, and the distal limb was placed in the BI (Fig. 1B).
Progress in the last 8 months has been favorable, with improvement of dyspnea, a 300ml increase in FEV1, resolution of respiratory failure, and no recurrence of obstructive episodes due to secretions to date (26 months post-transplantation).
Clinical Case 2A 56-year-old man who underwent bilateral LT in September 2012.
The patient developed fungal bronchitis in the immediate post-transplantation period that was successfully treated with antifungal agents. He had 2 episodes of acute rejection in months 2 and 6 post-transplantation, which responded well to treatment with steroids.
FB in the post-transplantation period revealed signs of fungal infection in the right anastomosis, with obstructive episodes due to secretions, progression of necrotic-appearing mucous membranes towards the BI and associated malacia, reducing the lumen to less than 20% on expiration.
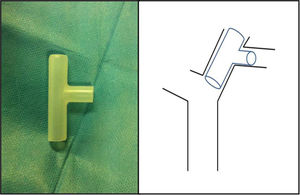
We decided to place a Montgomery stent (Fig. 2), caliber 11mm, distal limb 15mm, proximal limb 20mm, total length 46mm with a 10mm horizontal limb extending towards the RUL.
The patient's progress after stent placement was good, with clinical improvement and a 750ml increase in FEV1 1 month after the procedure. One year later, the patient remains free of complications.
DiscussionAirway complications are mainly caused by ischemia, since perfusion of the donor bronchus depends on pulmonary circulation via bronchial arteries that are generally not revascularized during surgery. However, other factors may also be involved, such as the surgical technique, primary graft dysfunction, lung infection before and after transplantation, acute graft rejection, intensive immunosuppression, prolonged mechanical ventilation and graft preservation.1
In both cases discussed here, the definitive treatment was placement of an appropriately adapted Montgomery stent. With this technique, BI stenosis could be treated, and right main bronchus malacia in the region of the bronchial anastomosis stabilized, maintaining RUL orifice patency. Endoscopic monitoring was performed 48h after the procedure in both cases, and then as required by the patients’ clinical status. Clinical and functional progress in both patients was good.
To date, only one article has been published on a series of 9 patients with LT and BI stenosis treated with a Montgomery or T-tube stent. FEV1 improved significantly after the procedure, while the most common complication was stent migration, reported in one third of the cases.3
In our patients, we were able to achieve good right bronchus patency, and problems such as obstructions due to secretion or migration were avoided. It seems likely that in the future, these cases will be treated with devices specifically designed for these sites, such as the recently developed Oki4 stent.
Please cite this article as: Pinillos Robles J, García Luján R, de Pablo Gafas A, de Miguel Poch E. Tratamiento de la estenosis de bronquio intermediario en el trasplante pulmonar con endoprótesis de Montgomery. Una técnica novedosa. Arch Bronconeumol. 2015;51:e5–e7.