Real-time elastography performed during endoscopic ultrasonography is a relatively new method for characterizing tissue stiffness, and has been used successfully as a predictor of malignancy in mediastinal lymph nodes.
This case report describes our practical experience with this technique using an ultrasound bronchoscope to examine mediastinal lymph nodes. We present a case of sectorial endobronchial ultrasound and the first published case of endoscopic ultrasound elastography using ultrasound bronchoscope in two patients with non-small cell lung carcinoma. Qualitative tissue color pattern was obtained in both cases and correlated with pathological evaluation.
The initial feasibility results are promising and suggest that ultrasound bronchoscopy techniques, such as guided nodal staging, merit additional studies. It may be important to categorize the risk of malignancy to facilitate sampling decisions.
La elastografía en tiempo real realizada durante la ultrasonografía endoscópica digestiva es una técnica relativamente nueva que permite caracterizar la dureza de los tejidos, y ha sido utilizada con éxito como predictor de malignidad en ganglios mediastínicos.
En la presente nota clínica se describe nuestra experiencia práctica en la técnica de la elastografía con ecobroncoscopio en el estudio de los ganglios linfáticos mediastínicos. Presentamos un caso realizado mediante ultrasonografía endobronquial sectorial y el primer caso publicado de elastografía por ultrasonografía endoscópica con ecobroncoscopio, en 2 pacientes con carcinoma de pulmón no microcítico. El patrón cualitativo en color del tejido se obtuvo en ambos casos y se correlacionó con la evaluación anatomopatológica.
Los resultados de viabilidad iniciales son prometedores y las aplicaciones ecobroncoscópicas, como la estadificación ganglionar guiada, requieren ser evaluadas. Categorizar el riesgo de malignidad puede ser importante para ayudar a tomar decisiones en la obtención de muestras.
Precise classification of lymph nodes as benign or malignant is essential for lung cancer staging. B-mode morphological ultrasound criteria for the detection of malignant lymph nodes during endobronchial ultrasound (EBUS) may be useful for predicting metastasis.1,2 However, inter- and intra-observer agreements for most sonographic signs are not sufficiently reliable.3 An alternative could be the use of endoscopic ultrasound elastography. With this technique, structural deformation caused by compression or vibration is mapped to produce color images representing the relative elasticity or stiffness of tissue. From these images, anomalies can be classified as benign or malignant. Only 1 previous publication4 on EBUS elastography is available, but this technique has been successfully applied in endoscopic ultrasound (EUS), with excellent inter-observer agreement.5
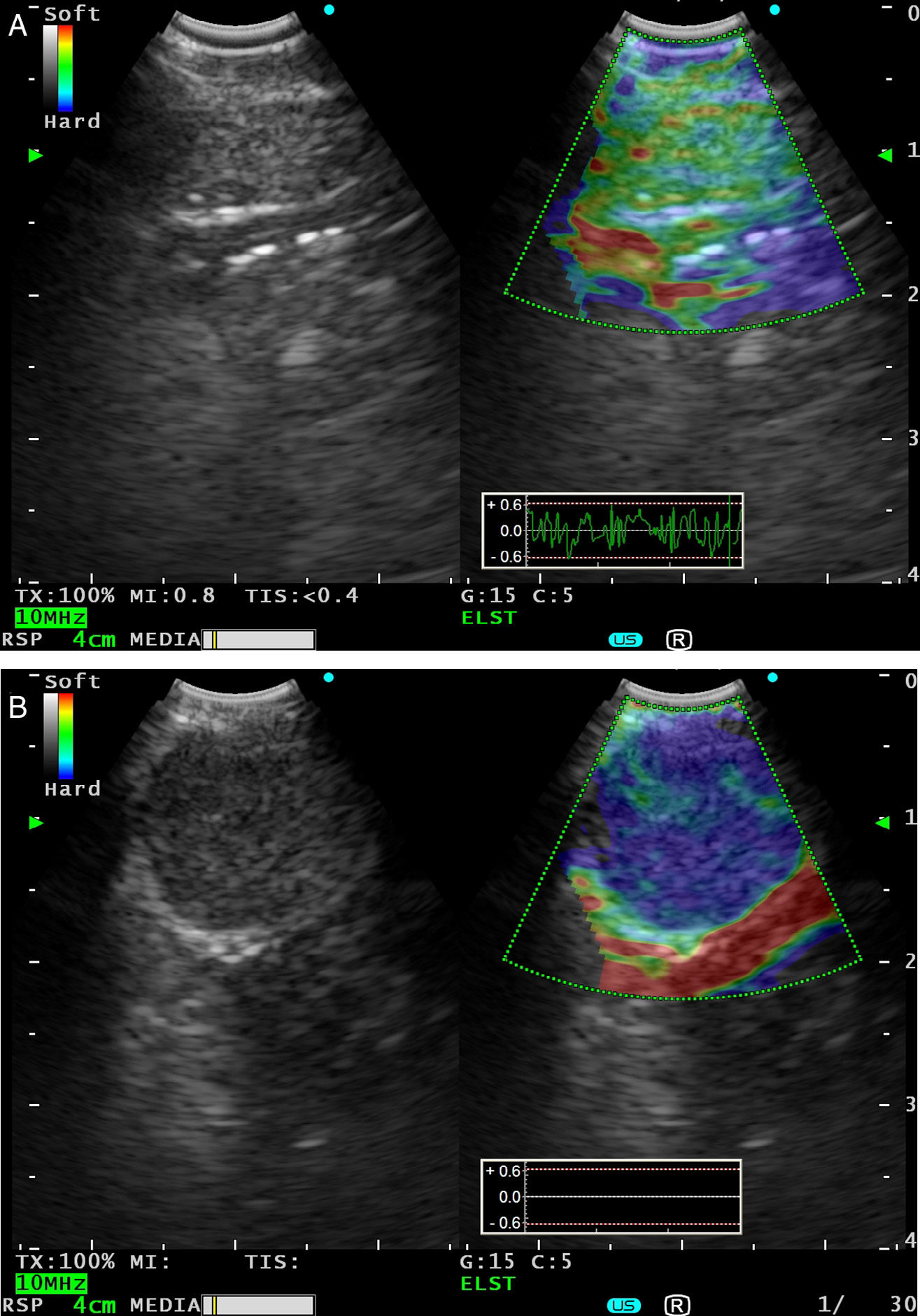
Case ReportsCase 1A 66-year-old man, former smoker for 4 years, with a history of moderate COPD and left pleural effusion and cytology negative for malignancy. In the previous 4 months, he had 2 episodes of left lower lobe (LLL) pneumonia. He presented in the emergency room with left pleuritic pain, increased cough and poor general condition. Positron emission tomography-computed tomography (PET-CT) revealed a hypermetabolic necrotic mass in the LLL and hypermetabolic left lower paratracheal, left subcarinal-paratracheal and left para-aortic lymphadenopathies, suggestive of metastasis. Bronchoscopy was performed, showing endobronchial tumors in LLL segment 10. Bronchial brushing cytology showed squamous cell carcinoma. EBUS (BF-UC180F Olympus, Japan) was performed, with aspiration of lymph node stations 4R-1 (5.4mm), 4R-2 (5.9mm), 4R-3 (7.5mm), 7-1 (6.6mm×21.4mm), 4L-1 (13.1mm×15.4mm) and 7-2 (12.6mm×15.5mm) after a change of needle. Lymph node stations 7-1 and 7-2 were examined using elastography (EU-ME2 Premier Plus Olympus processor, Japan), obtaining a qualitative pattern of color images showing tissue areas with greater consistency in dark blue, intermediate in green and the softest in red (Fig. 1A and B). In double-screen mode, the B-mode image is on the left, and on the right, the color-coded image of stiffness responses is superimposed on the B-mode image. The region of interest for the elastography calculations was selected manually, with inclusion of the node station and adjacent tissues. Aspirates were negative for malignancy, with the exception of stations 4L-1 and 7-2, that returned a diagnosis of squamous cell carcinoma and tumor necrosis.
(A) Conventional black and white EBUS B-mode image (left) and with real-time EBUS elastography (right), showing a 6.6mm benign subcarinal lymph node, seen as an area of intermediate rigidity (green). (B) EBUS elastography (right) showing a 12.6mm malignant subcarinal lymphadenopathy, seen as a stiff area (dark blue-cyan), due to squamous cell carcinoma infiltration.
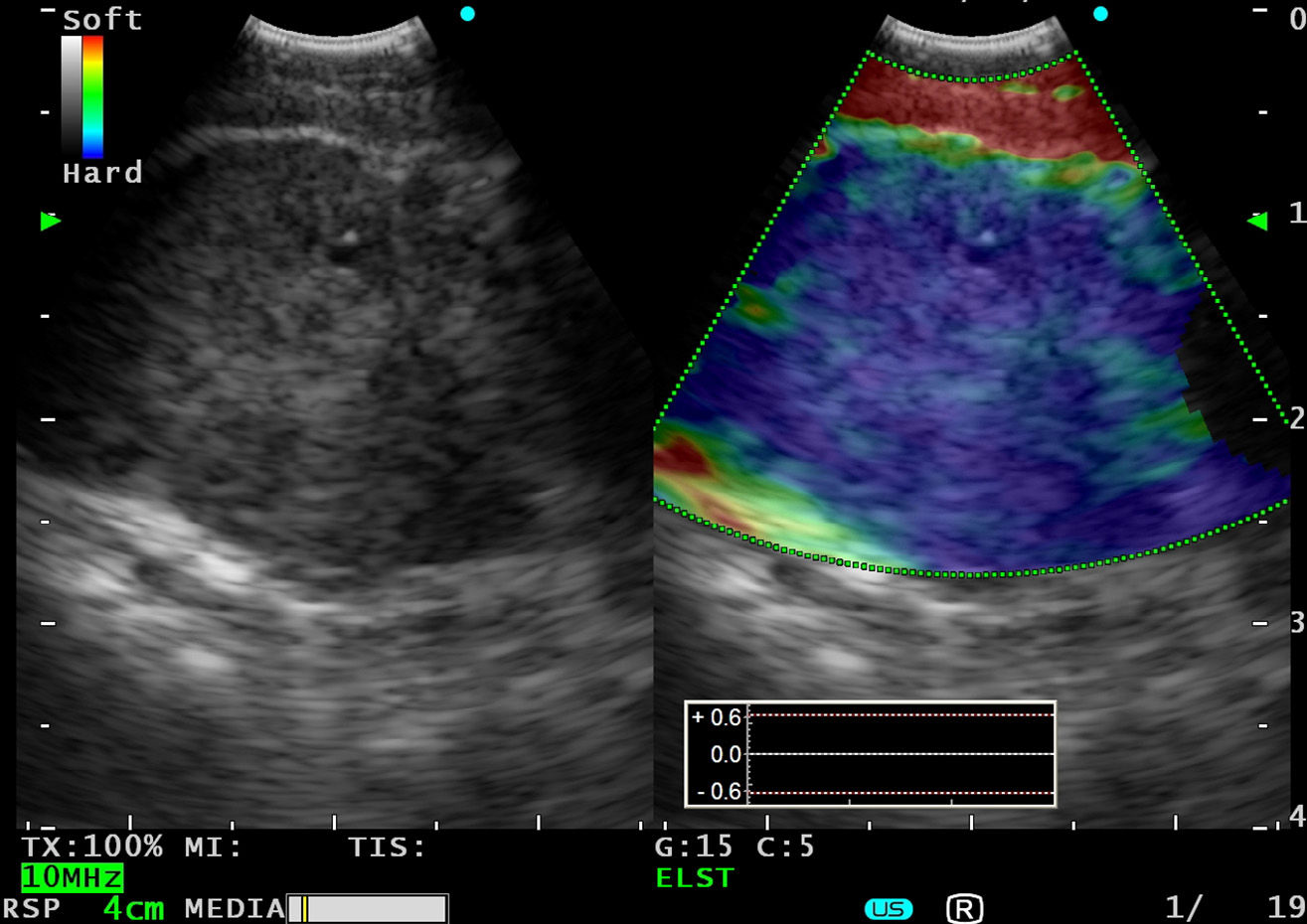
A 74-year-old male smoker with hypertension, dyslipidemia, previous acute myocardial infarction and polycythemia. He reported a 45-day history of progressive dysphonia and a sensation of instability for 3–4 months that had intensified in the previous few days, to the stage that he could no longer stand. The chest CT showed a pulmonary nodule measuring 2cm in the right upper lobe, suggestive of primary pulmonary neoplasia, multiple small bilateral pulmonary nodules suggestive of metastasis, and multiple enlarged mediastinal lymph nodes. A head CT revealed radiological signs indicative of multiple cerebral metastases. Due to significant cerebral edema,6 ultrasound-guided bronchoscopy with esophageal access was performed under conscious sedation with midazolam. A 20mm subcarinal lymphadenopathy was visualized and aspirated. Elastography mode indicated that the consistency of this nodule was significantly increased (Fig. 2). The diagnosis was metastatic lung adenocarcinoma.
DiscussionElastography can improve the diagnostic yield of EUS-guided fine needle aspiration by discriminating between benign and malignant nodes.7,8 It may also be useful for identifying malignant areas in lymphadenopathies with uneven disease involvement, and for guiding the aspiration needle toward those areas. In a recent metaanalysis, EUS elastography was calculated to have a sensitivity of 88% and a specificity of 85% for differentiating between benign and malignant lymph nodes.9
In the case of tracheobronchial access, the technique may be limited by the consistency and irregular surface of the cartilages and difficulty in applying pressure with the distal tip of the ultrasound-guided bronchoscope. In our first EBUS case, fixed elastographic images were obtained from a dynamic sequence adjusted for elasticity analysis. This analysis was consistent with the cytological results of the aspirates. Esophageal access with ultrasound-guided bronchoscopy was equally free of limitations. Tissue artifacts from breathing or cardiac movements probably caused the nodes to shift with respect to the bronchial or esophageal wall and the transducer.
To conclude, elastography is a viable technique for the characterization of tissues during EBUS that may help predict malignancy in lymph nodes and improve specimen recovery. Further studies evaluating the usefulness of EBUS elastography in large series of patients are needed.
FundingThis study was partially funded by a SEPAR2010 grant.
Conflict of InterestsThe authors declare that they have no conflict of interests.
Please cite this article as: Andreo García F, Centeno Clemente CÁ, Sanz Santos J, Barturen Barroso Á, Hernández Gallego A, Ruiz Manzano J. Experiencia inicial con elastografía en tiempo real mediante ecobroncoscopio en la evaluación de ganglios linfáticos mediastínicos. Arch Bronconeumol. 2015;51:e8–e11.