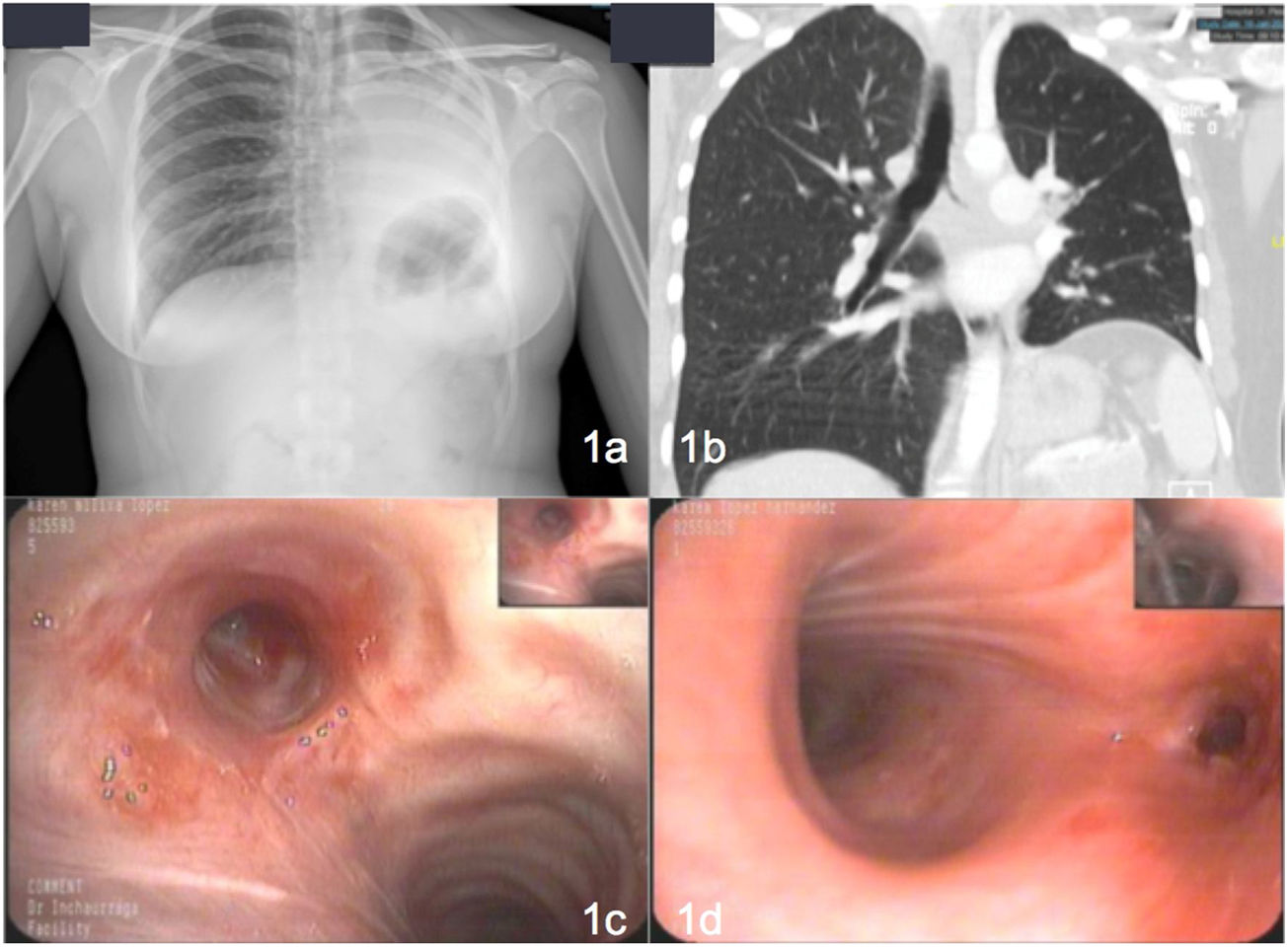
Our patient was a 24-year-old woman with a previous diagnosis of pulmonary tuberculosis. After 4 months of treatment with rifampicin+isoniazid and 2 months with rifampicin+isoniazid+pyrazinamide+ethambutol with good adherence, she showed clinical improvement, radiological improvement, and negative sputum smear microscopy and culture. She presented due to sudden onset of dyspnea, pleuritic chest pain, and desaturation. X-ray was performed (Fig. 1a), revealing consolidation with atelectasis of practically the entire left lung. Chest computed tomography (CT) (Fig. 1b) showed complete occlusion of the lumen with occupation extending to the anterior segmental bronchus, the lingula, and the left lower lobe with secondary atelectasis. Stenosis was confirmed by bronchoscopy (Fig. 1c and d) and a diagnosis of endobronchial tuberculosis was confirmed by lung biopsy. Cryotherapy and corticosteroid therapy were administered, leading to clinical improvement and partial improvement of the obstruction. Bronchoscopy with balloon dilation was performed, resolving the atelectasis.
(A) Chest X-ray showing condensation with atelectasis of virtually the entire left lung. (b) Complete occlusion of the lumen with occupation extending to the anterior segmental bronchus, the lingula, and the left lower lobe with secondary atelectasis. (c and d) Mucosal thickening with some nodular appearance partially obstructing the entrance to the left main bronchus preventing passage of the bronchoscope, so lobar bronchi are not visualized.
Tracheobronchial tuberculosis can produce stenosis of the trachea or bronchi, atelectasis, post-obstructive pneumonia, hemoptysis, chest pain, and dyspnea.1,2 CT can be used to evaluate and diagnose endobronchial lesions and determine the degree of stenosis, while bronchoscopy is useful for evaluating possible causes. Treatment may involve corticosteroids, but in case of severe stenosis, endoscopic or surgical dilation techniques may be required.1,2