We report the case of a 56-year-old man who presented with a 2-week history of dyspnea (mMRC grade 3/4), facial edema, distended neck veins, and headache.
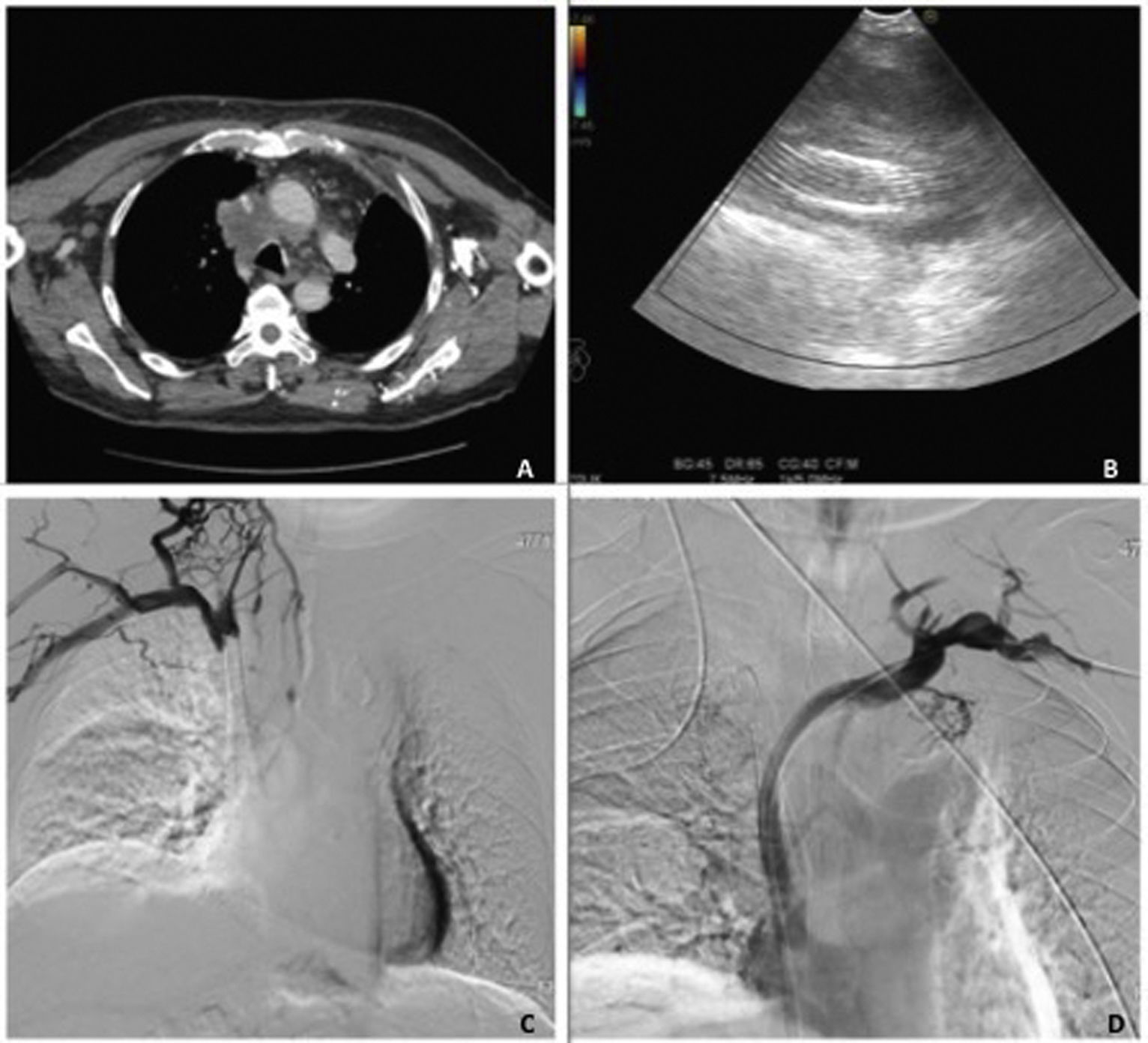
Additional tests revealed the presence of a right paratracheal lymph node cluster with extrinsic compression of the superior vena cava (Fig. 1A), so we decided to implant a stent and to start treatment with enoxaparin, acetylsalicylic acid, and clopidogrel.
(A) Chest CT (axial slice, mediastinal window): right paratracheal lymph node cluster with extrinsic compression of the superior vena cava. (B) Endobronchial ultrasound, Doppler-mode analysis showing lymph node cluster with elongated hyperechoic image (stent), containing no evidence of blood flow. (C) Superior vena cavogram showing no passage of contrast agent through the stent, consistent with stent thrombosis. (D) Superior vena cavogram showing complete recanalization after new stent placement.
The patient's symptoms resolved, and an endobronchial ultrasound was performed after withdrawal of enoxaparin and clopidogrel. This revealed a lymph node cluster in the 4R mediastinal territory, containing an elongated hyperechoic image with posterior enhancement, consistent with the previously placed stent. Doppler-mode analysis showed an absence of blood flow through the stent (Fig. 1B). Stent thrombosis was suspected, so superior vena cavogram was performed, which confirmed the endoscopic findings (Fig. 1C). A new stent had to be implanted to achieve complete recanalization (Fig. 1D).
Endobronchial ultrasound, therefore, facilitated a histological diagnosis and provided evidence of vena cava stent thrombosis in the same procedure. Given the low hemorrhagic risk of the procedure,1,2 an individualized risk-benefit assessment of maintaining antiplatelet therapy may be made, in order to reduce the thrombotic risk.
Authorship of this article was limited, so we would like to express our thanks to the interventional radiology department of the Hospital Clínico Universitario Valladolid.