The patient's position during an axillary thoracotomy can cause postoperative pain and decrease mobility of the ipsilateral shoulder. In this study, we assessed whether the implementation of a standardized analgesia program using transcutaneous electrical nerve stimulation (TENS) decreases local pain and improves ipsilateral shoulder mobility.
MethodRandomized, single-blind, single-center clinical trial of 50 patients who had undergone anatomical lung resection via axillary muscle-sparing thoracotomy. Patients were treated with TENS devices for 30min every 8h, beginning on postoperative day 1. Pain and mobility of the affected limb were recorded at the same time on postoperative days 1 through 3. A visual analog scale was used for pain assessment and shoulder mobility was assessed with a goniometer. Results were compared using a non-parametric test.
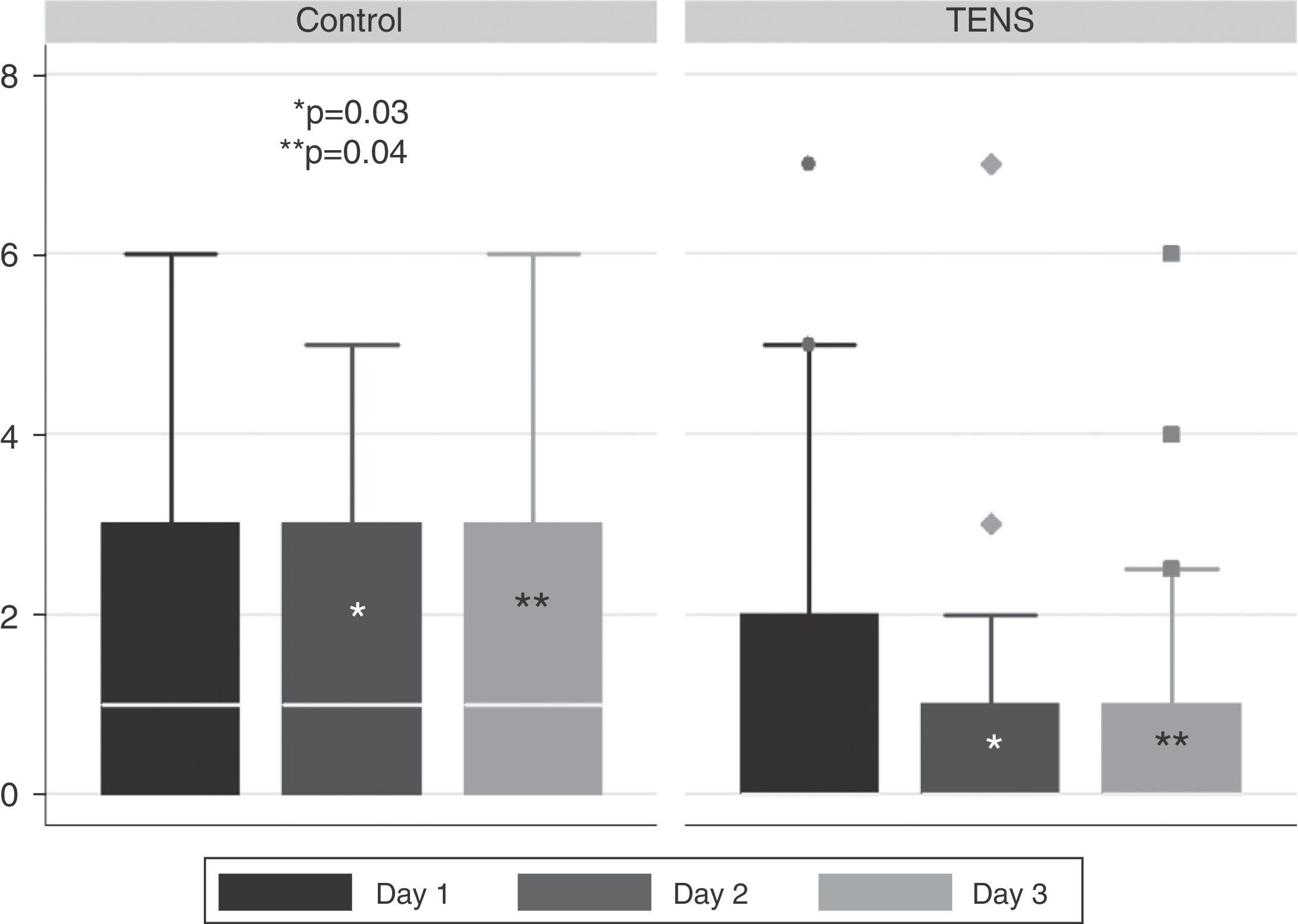
ResultsTwenty-five patients were randomized to each group. Mean age of the control group was 62.7±9.3 years and 63.4±10.2 years in the experimental group. Shoulder mobility parameters were similar in both groups on all postoperative days. However, pain during flexion significantly decreased on day 2 (P=.03) and day 3 (P=.04) in the experimental group.
ConclusionThe use of TENS decreases pain from shoulder flexion in patients undergoing axillary thoracotomy for pulmonary resection.
La posición del paciente durante la toracotomía axilar puede producirle alteraciones postoperatorias por dolor y disminución de la movilidad del hombro. En este estudio pretendemos evaluar si la aplicación de un programa estandarizado de analgesia mediante estimulación eléctrica transcutánea (TENS) disminuye el dolor e incrementa la recuperación de la movilidad de la articulación del lado intervenido en estos pacientes.
MétodoEnsayo clínico monocéntrico aleatorizado simple ciego, en pacientes sometidos a resección pulmonar por minitoracotomía axilar sin sección muscular. Los pacientes fueron tratados durante 30min cada 8h con dispositivos TENS, desde el día siguiente a la intervención. Se realizaron registros del dolor y movilidad del miembro afectado todos los días a la misma hora durante los primeros 3 días postoperatorios. Para evaluar el dolor se utilizó una escala visual analógica, y para valorar la movilidad del hombro, un goniómetro. Los valores obtenidos se compararon entre los 2 grupos mediante un test no paramétrico.
ResultadosSe han incluido 50 casos, 25 en el grupo experimental y 25 en el grupo control. La edad media del grupo control es de 62,76años, y la del grupo expuesto, de 63,4años. No se han obtenido diferencias significativas en la movilidad del hombro en ninguno de los días postoperatorios. El dolor a la flexión del hombro durante los días segundo (P=0,03) y tercero (P=0,04) fue significativamente menor en los pacientes del grupo experimental.
ConclusionesEl uso de TENS disminuye el dolor a la flexión del hombro en pacientes sometidos a toracotomía axilar para resección pulmonar.
Post-operative pain increases patient suffering, and can cause physiopathological changes that can increase the rate of post-operative complications, delay recovery, and increase hospital costs. The first consensus document on post-operative pain published in Spain in 20051 defines post-operative pain as pain that appears as a consequence of the surgical procedure. However, it is also often refered as pain occuring in a surgical patient caused by previous disease, the surgical procedure itself, or a combination of both.
Post-thoracotomy shoulder pain is typically ipsilateral, periarticular, diffuse, and independent from pain caused by the thoracotomy. The origin has not yet been determined, but it has been associated with direct muscle damage caused by the thoracotomy, pleural irritation produced by the surgical procedure, and reactivation of previous joint injuries.2 Up to 75% of thoracotomy patients report moderate to severe pain, despite receiving epidural analgesia in the immediate post-operative period.3
Several different methods are available for pain control, consisting mainly of pharmacological treatment, nerve blocks, and other non-pharmacological techniques, such as relaxation, acupuncture, hypnosis, and transcutaneous electrical nerve stimulation (TENS). Nonetheless, despite more-or-less standardized use of these analgesic resources, particularly pharmacological treatment, patients’ immediate post-operative quality of life continues to be diminished by shoulder pain.
In this single-blind, randomized study, we investigated the efficacy of TENS in reducing post-thoracotomy ipsilateral shoulder pain and improving the functional recovery of the joint.
MethodsDesignThis was a single-blind, randomized study conducted in patients undergoing muscle-sparing axillary thoracotomy for lung resection in the Thoracic Surgery Department of the University of Salamanca.
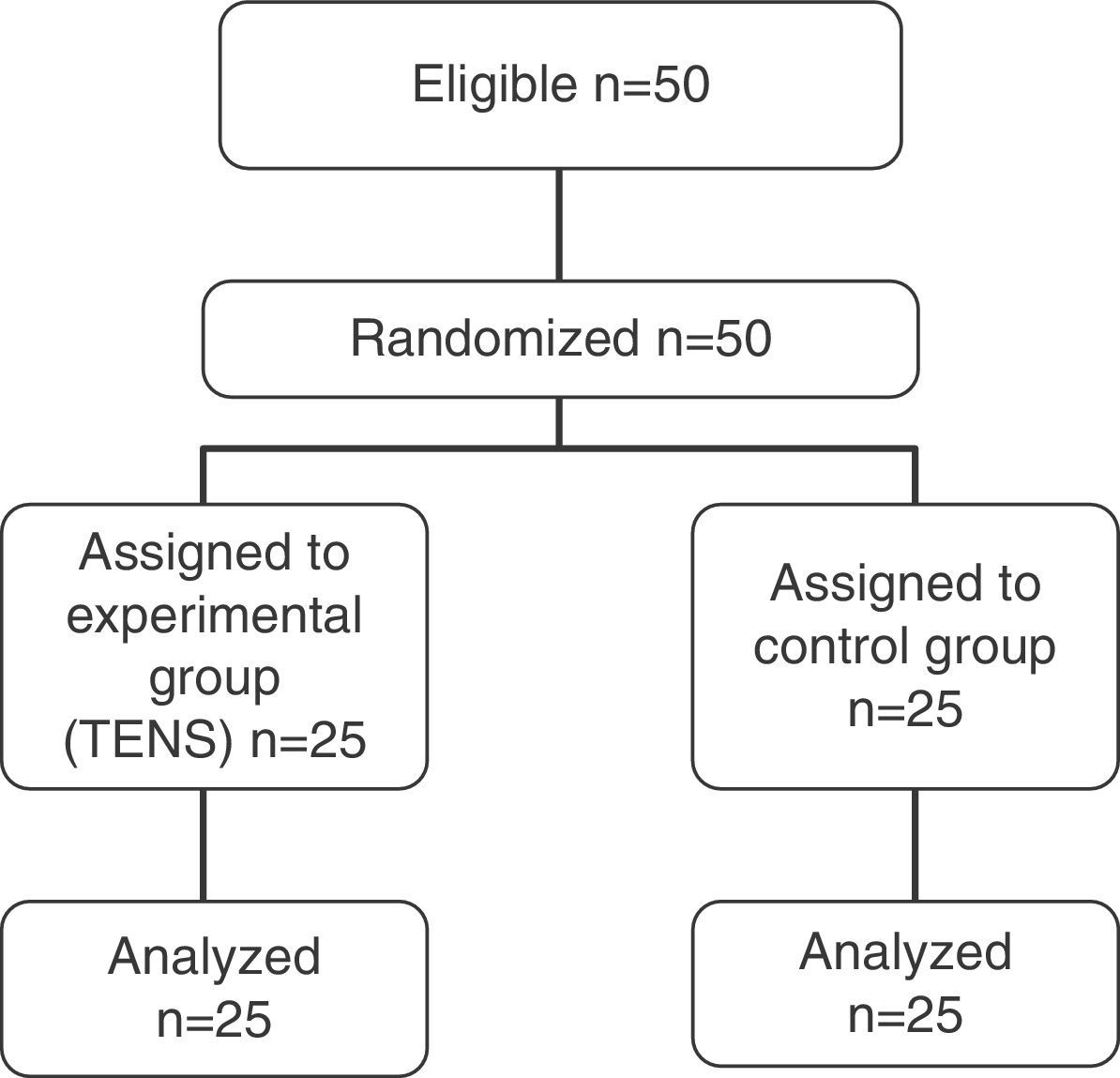
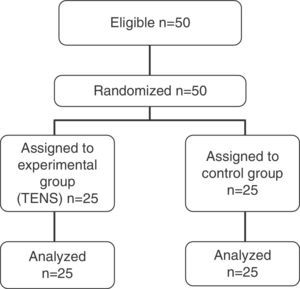
PopulationA total of 50 patients scheduled for lung resection between February 2013 and October 2013 were prospectively included in this study (Fig. 1). The cases were selected according to the following criteria: patients scheduled for major lung resection who did not require wall resection, who underwent muscle-sparing axillary resection. Exclusion criteria included: previous chemotherapy or radiation induction treatment, previous joint disease that would impede normal shoulder joint mobility and contraindications for the use of TENS, for example, patients with pacemakers or surgical wound infection. Patients were selected by the department's surgeons during the outpatient consultation held prior to admission. The hospital ethics committee approved the study and all patients signed informed consent for participation.
Before anesthesia was induced, an epidural catheter for intraoperative and post-operative analgesia was placed at D5–D7 level. Analgesia was administered in the form of ropivacaine 0.2%, 6–8ml/h in continuous infusion via the catheter, combined with administration every 8h of paracetamol and a non-steroidal anti-inflammatory drug (NSAID) (ibuprofen) or metamizole, depending on the patient's possible allergic status. The epidural catheter was removed 48h after the intervention. Some patients received oral tramadol 50mg every 8 or 12h after catheter removal.
Positioning of the patient on the table was standardized: lateral decubitus, resting on the non-affected side, thus procuring a cleavage zone at the level of the xiphoid apophysis; the resting arm was placed on an arm board, with the wrist flexed and secured in a safe position; the arm on the side of the intervention was abducted at 90° with the elbow flexed at 90°–100°. This arm was supported by straps once straining of the shoulder was ruled out and correct positioning of the hand was ensured in order to prevent radial nerve injuries (Fig. 2).
After the surgical procedure, all patients were extubated on the operating table and transferred to the post-operative recovery room, where post-operative physiotherapy exercises were started, as proposed by Varela et al.4 Twenty-four hours after the procedure, all patients were out of bed, walking and performing 15min of aerobic exercise on the unloaded cycle ergometer twice a day.
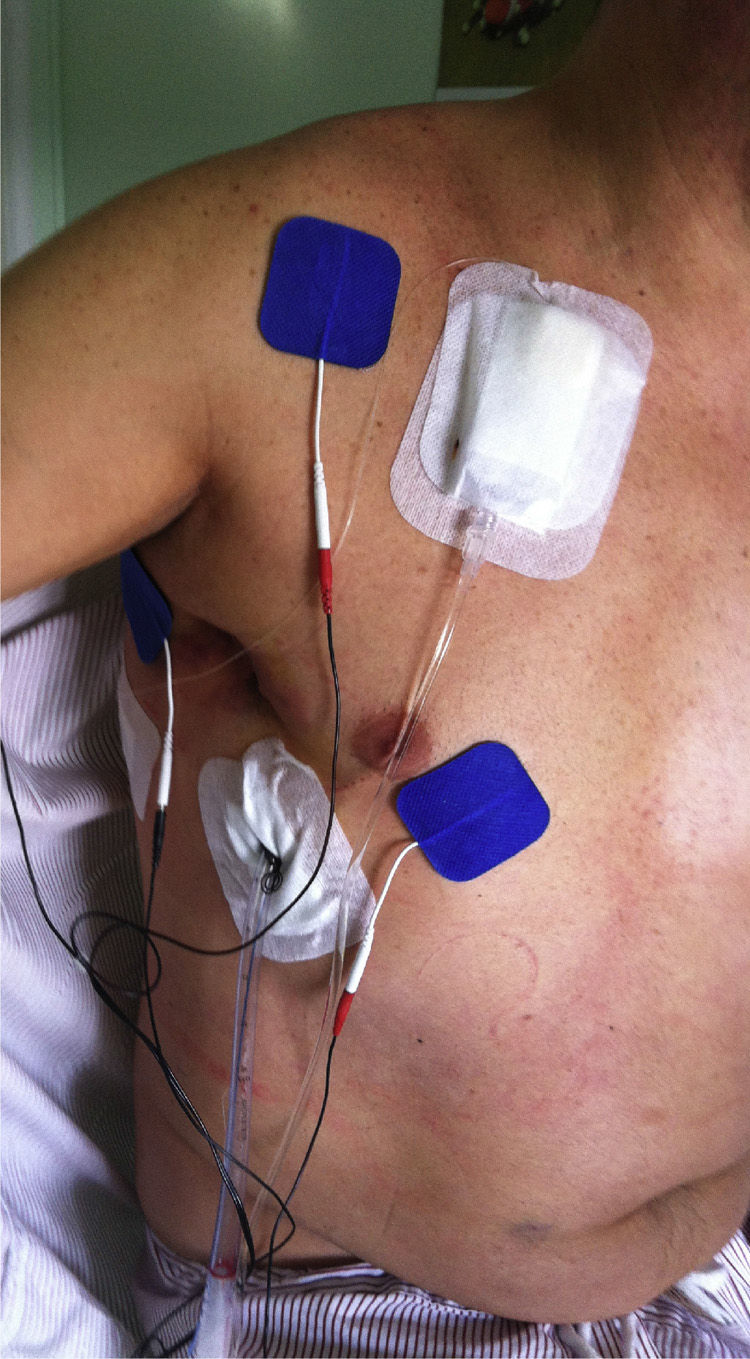
MaterialsApex® DIGI-COMBO equipment was used for this study. These devices provide an asymmetric biphasic waveform at a frequency of 80Hz and a pulse width of 120μs. Four reusable 50cm×50cm self-adhesive, latex-free carbon film electrodes with long-lasting gel (Key Life S.L.) were placed as follows: 1 electrode on either side of the surgical incision (2cm from the wound) and 2 on the shoulder, one on the anterior aspect and the other on the posterior aspect (Fig. 3).
Randomization and Treatment ProtocolOn the day of admission to the hospital for the intervention, patients were assigned to the experimental or control group according to a series of random numbers generated by Excel®. The numbers were retrieved in such a way that the assignation of the following patient was unknown until the time of admission.
During the study period, patients followed the same general perioperative physiotherapy protocol,4 which does not include specific active-assisted mobilization of the shoulder. The TENS electrostimulation protocol for both groups consisted of 30-min sessions every 8h, starting on the day following surgery. Patients in the control group were treated with a device that was identical to the standard device but manipulated to disable the pulse. The study physiotherapist was responsible for pre- and post-operative procedures and for placing the TENS electrodes.
Study VariablesThe following demographic variables were recorded to characterize the study population: age, sex, weight and height.
At the time of admission, all patients underwent an initial evaluation, consisting of a study of the affected shoulder. Range of motion, internal and external rotation, and abduction were measured by goniometer, and pain intensity for each movement was determined on a 100mm visual analog scale (VAS: range 0–10).
Starting 24h after surgery, pain, mobility of the affected shoulder, according to goniometer, and VAS measurements were recorded at the same time every day, during the first 3 days. Study variables included shoulder pain and the degrees of flexion, internal and external rotation and abduction recorded for the shoulder ipsilateral to the surgery.
Data AnalysisA descriptive, comparative analysis was performed using parametric and non-parametric tests of demographic and study variables, as appropriate, after analyzing for normal distribution. Comparative studies were performed using parametric or non-parametric tests depending on the distribution of the variable under study. Statistical analysis was performed using Stata 12.1 software.
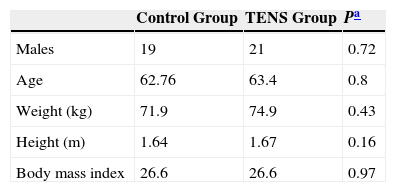
ResultsA total of 50 patients was included, 25 in each study group. The demographic characteristics of each group were statistically similar (Table 1). It is interesting to note that 80% of patients in the series were men. All 50 patients completed the treatment protocol and none suffered any complications, intolerance or other problems that might have required suspension of the TENS intervention.
Demographic Data of Study Patients.
| Control Group | TENS Group | Pa | |
|---|---|---|---|
| Males | 19 | 21 | 0.72 |
| Age | 62.76 | 63.4 | 0.8 |
| Weight (kg) | 71.9 | 74.9 | 0.43 |
| Height (m) | 1.64 | 1.67 | 0.16 |
| Body mass index | 26.6 | 26.6 | 0.97 |
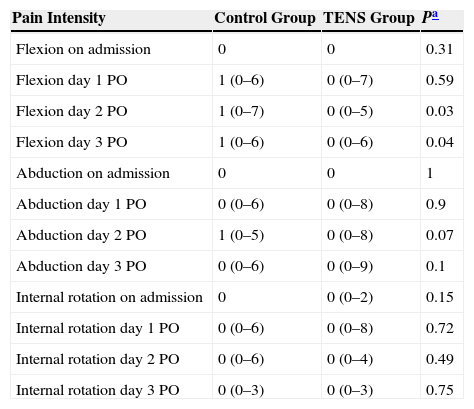
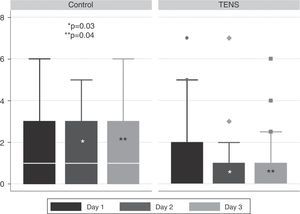
Pain and shoulder mobility after the intervention were similar in both groups (Tables 2 and 3), except for pain intensity on flexion on post-operative days 2 and 3, which was significantly less in patients in the experimental group (Fig. 4).
Post-Thoracotomy Pain on Moving the Ipsilateral Shoulder on Day of Admission and on the First 3 Post-Operative (PO) Days (Mean and Range).
| Pain Intensity | Control Group | TENS Group | Pa |
|---|---|---|---|
| Flexion on admission | 0 | 0 | 0.31 |
| Flexion day 1 PO | 1 (0–6) | 0 (0–7) | 0.59 |
| Flexion day 2 PO | 1 (0–7) | 0 (0–5) | 0.03 |
| Flexion day 3 PO | 1 (0–6) | 0 (0–6) | 0.04 |
| Abduction on admission | 0 | 0 | 1 |
| Abduction day 1 PO | 0 (0–6) | 0 (0–8) | 0.9 |
| Abduction day 2 PO | 1 (0–5) | 0 (0–8) | 0.07 |
| Abduction day 3 PO | 0 (0–6) | 0 (0–9) | 0.1 |
| Internal rotation on admission | 0 | 0 (0–2) | 0.15 |
| Internal rotation day 1 PO | 0 (0–6) | 0 (0–8) | 0.72 |
| Internal rotation day 2 PO | 0 (0–6) | 0 (0–4) | 0.49 |
| Internal rotation day 3 PO | 0 (0–3) | 0 (0–3) | 0.75 |
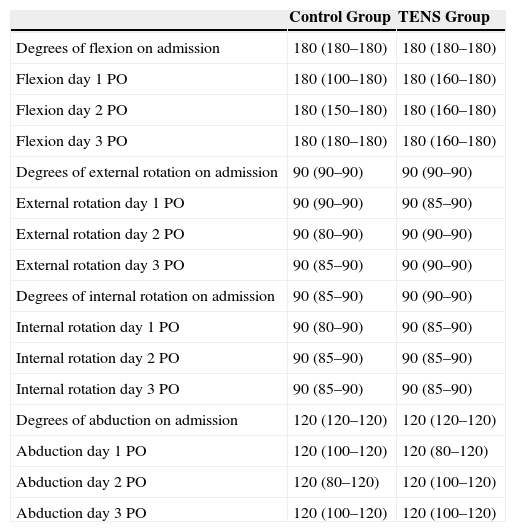
Degrees of Mobility Achieved in Shoulder Ipsilateral to Thoracotomy on Day of Admission and 3 Initial Post-Operative (PO) Days (Mode and Range).
| Control Group | TENS Group | |
|---|---|---|
| Degrees of flexion on admission | 180 (180–180) | 180 (180–180) |
| Flexion day 1 PO | 180 (100–180) | 180 (160–180) |
| Flexion day 2 PO | 180 (150–180) | 180 (160–180) |
| Flexion day 3 PO | 180 (180–180) | 180 (160–180) |
| Degrees of external rotation on admission | 90 (90–90) | 90 (90–90) |
| External rotation day 1 PO | 90 (90–90) | 90 (85–90) |
| External rotation day 2 PO | 90 (80–90) | 90 (90–90) |
| External rotation day 3 PO | 90 (85–90) | 90 (90–90) |
| Degrees of internal rotation on admission | 90 (85–90) | 90 (90–90) |
| Internal rotation day 1 PO | 90 (80–90) | 90 (85–90) |
| Internal rotation day 2 PO | 90 (85–90) | 90 (85–90) |
| Internal rotation day 3 PO | 90 (85–90) | 90 (85–90) |
| Degrees of abduction on admission | 120 (120–120) | 120 (120–120) |
| Abduction day 1 PO | 120 (100–120) | 120 (80–120) |
| Abduction day 2 PO | 120 (80–120) | 120 (100–120) |
| Abduction day 3 PO | 120 (100–120) | 120 (100–120) |
Compared using Mann–Whitney U test. All comparisons were statistically insignificant (P>.9).
In this study, we investigated shoulder pain relief and dynamic functional recovery analyzing shoulder joint movements: flexion, abduction and external and internal rotation. The results indicated that TENS is only useful from post-operative day 2 onwards, and specifically for flexion movements. However, we found that the reduction in the pain scale for this movement was clinically relevant, since it speeds up recovery of normal upper limb activity necessary for a multitude of activities of daily living.
The origin of post-thoracotomy pain has yet to be fully clarified. It has been related with various mechanisms and specific treatments have been suggested for each of these. The different theories can be grouped into 2 contrasting hypotheses: in one, post-thoracotomy pain is associated with pain from pleural inflammation mediated by the phrenic nerve2,5–8; in the other, it is the result of perioperative damage or reactivation of a previous shoulder injury.2,9–12 Pain mediated by the phrenic nerve is a result of the surgical procedure, therefore, epidural analgesia should be effective. Pain associated with joint lesions, however, should not respond to epidural analgesia but to NSAIDs or other medical intervention. In our study, all patients recieved epidural analgesia and anti-inflamatory drugs. Despite these inteventions patients reported pain on mobilization of the shoulder. The muscles of the chest wall (latissimus dorsi, serratus anterior, and pectoral muscles) play an important role in the mobility of the arm, so there is little doubt that any insult to this region will have a significant impact on the degree of pain and functional limitation of the shoulder.13 Bearing in mind the type of thoracotomy performed in our study, changes in functionality can only be associated with injury to the serratus anterior, which inserts into and stabilizes the scapula and is essential for upper limb flexion. We found that TENS was effective in relieving the pain caused by this movement. This analgesia technique is known to work by inhibiting the central transmission of nociceptive impulses sent by slow unmyelinated fibers using the overstimulation produced by a faster-traveling impulse transmitted via myelinated fibers. This is known as the gate-control theory.14
The level of pain reported by patients may occasionally be high, since it ranges between 0 and 6, even on post-operative day 3. Although it mainly occurs on flexion, some patients report pain, albeit of lower intensity, when performing other movements (Table 2). This pain is unrelated to muscle injury occurring during surgery, so must be attributable to one of the other proposed theories.
Several studies have evaluated the effectiveness of TENS in pain relief. Many of these were designed to evaluate waning requirements for analgesia in the presence of musculoskeletal pain. Johnson and Martinson15 recently published a meta-analysis on the efficacy of TENS in reducing chronic musculoskeletal pain at any site. They looked at 38 studies with a total of 1227 patients and found a very significant reduction in pain (P<.0005) in individuals who received TENS compared with placebo. Singling out studies on post-thoracotomy pain, we also find evidence16–20 supporting the efficacy of TENS in reducing pain in the affected hemithorax, a reduced need for analgesia, and improvements in other parameters, such as respiratory function. Although most studies show benefits, others have reported little effect and results similar to other treatments. Stubbing and Jellicoe21 did not find statistically significant differences in the need for oral analgesia or in peak-flow measurements between the experimental groups receiving TENS and control groups. Benedetti et al.22 conducted a study in 324 patients undergoing surgical procedures of different types. They concluded that TENS was not effective in the group that underwent posterolateral thoracotomy, but that it was useful in other thoracic procedures, such as median sternotomy and video-assisted thoracoscopy causing mild to moderate pain. Similarly, Freynet and Falcoz23 subsequently found that TENS alone was not effective as pain control after posterolateral thoracotomy, but that it was very useful in the management of pain after muscle-sparing mini-thoracotomy or after video-assisted procedures. These authors reported a reduction in need for narcotic painkillers, improvements in forced vital capacity parameters, and improved grades of chest and shoulder mobilization.
Despite an exhaustive search, we were unable to locate any reports specifically analyzing the efficacy of TENS in post-thoracotomy shoulder pain, and we were unable to compare our results with those of other published studies. From this, we can conclude that this is the first study of its kind. We would like to emphasize one aspect of our study in particular: the range of joint mobility observed among our patients remains largely unchanged after post-operative day 1. Reeve et al.24 in a randomized study analyzed the influence of perioperative physiotherapy on shoulder mobilization, among other parameters. Patients in the experimental group carried out physiotherapy exercises specifically targeting the shoulder as part of a wider intervention protocol. Exercises were started before surgery and continued into the immediate post-operative period, and patients were instructed to continue them after discharge. After analyzing the data, the authors concluded that the inclusion of a targeted physiotherapy program improves general pain and specifically shoulder pain, but they found no differences between the groups in range of movement or strength of the upper limb, or overall quality of life. Comparing their tables with our data, we found that the range of movement of their patients was remarkably more limited than ours (Table 3). We can offer no clear explanation for this finding, other than that it may be related with the general analgesic regimen used in our study; Reeve et al.24 do not specify the given analgesia.
Our study has some limitations that should be mentioned. Firstly, our sample size is small. However, this is a randomized, patient-blinded study, and as the groups are similar, the conclusions are very robust. The second limitation is a slight variability in the positioning of patients on the operating table. Variations in this variable are inevitable, unless the same person positions the patient every time, and this may affect the degree of pain experienced by the patient in the post-operative period. The third limitation to take into account is subjectivity in the perception and manifestation of pain. This issue may not be fully resolved but the visual analog scale for pain is a widely validated method.
To conclude, the use of TENS reduces pain on flexion of the shoulder in patients undergoing axillary thoracotomy, and this method has now been included in the post-operative management of our patients. Further research could explore whether this outcome affects patients’ post-operative quality of life, since shoulder flexion is involved in the majority of activities of daily living.
Conflict of InterestsThe authors state that they do not have any conflict of interest that could cause any bias in relation to this work.
Please cite this article as: Esteban González P, Novoa NM, Varela G. La estimulación nerviosa transcutánea disminuye el dolor del hombro ipsilateral postoracotomía. Estudio prospectivo aleatorizado. Arch Bronconeumol. 2015;51:621–626.