We report the case of a 53-year-old man, non-smoker, monitored for Crohn’s disease of the ileum by the digestive diseases department from the age of 14 years. Ileocecal resection was performed more than 20 years previously. He has been receiving mercaptopurine for 12 years and infliximab for 6 years, and has had no flare-ups in the last 10 years.
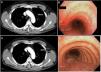
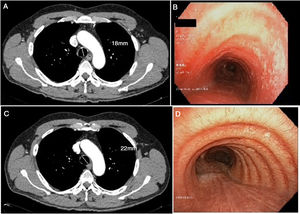
He was referred to our clinic with a 1-month history of non-productive cough and fever. During the course of these symptoms, he received 2 antibiotic regimens, first with levofloxacin and then with amoxicillin-clavulanate. The chest X-ray showed no significant changes and pulmonary function tests were significant only for slightly altered diffusion results (FEV1 3,100 [91%]; FVC 3,550 [81%]; FEV1/FVC 87%; DLCO 71%; KCO 101%). Given the suspicion of infectious disease in an immunosuppressed patient, azithromycin was added to the treatment plan, and a computed axial tomography (CT) scan was performed, which revealed discreet tracheal wall thickening, with no evidence of pulmonary consolidations or other type of involvement (Fig. 1). The bronchoscopy was significant for raised whitish lesions in the tracheal wall and at the entrance of the two main bronchi, predominantly in the posterior tracheal wall (Fig. 1). An opportunistic infection was suspected, so bronchoalveolar lavage (BAL) was performed and samples were sent to the microbiology lab: standard pathogen panel (bacteria, mycobacteria, fungi, viruses, etc.) was negative. The pathology study of the tracheal wall biopsy reported nonspecific inflammatory signs with areas of ulceration. BAL cellularity consisted mainly of macrophages (80%), lymphocytes (15%) and polymorphonuclear cells (5%).
(A) Cross-sectional chest CT slice showing tracheal thickening, including measurement of the tracheal diameter. (B) Pre-treatment bronchoscopy showing lesions in the tracheal wall. (C) Cross-sectional CT slice following treatment with inhaled corticosteroids. (D) Bronchoscopy with no lesions after treatment, including measurement of the tracheal diameter.
A diagnosis of tracheobronchitis due to Crohn’s disease was given. Treatment started with inhaled corticosteroids (fluticasone 1,000 mg every 12 h). After 1 month of treatment, the patient's symptoms had disappeared, so dosing was reduced to 500 mg every 12 h. A chest CT scan was repeated, in which chest wall thickening was no longer visualized. Bronchoscopy after treatment confirmed the resolution of the earlier lesions.
Extraintestinal manifestations may occur in 6%–47% of patients with inflammatory bowel disease.1 Pulmonary involvement is an infrequent event, although underdiagnosis is common in many cases, and it has been suggested that it might occur in up to 60% of patients with inflammatory bowel disease1; the most characteristic manifestation is ulcerative colitis. The entire respiratory system may be involved, from the upper airway to the pulmonary parenchyma. Bronchiectasis is the manifestation most often described in the literature: some series report this type of involvement in up to 66% of cases.1–3 Tracheobronchitis in Crohn's disease is very rare and often accompanied by inflammatory bowel disease in remission.4,5
These manifestations tend to occur in the fifth decade of life and appear after diagnosis of inflammatory bowel disease in more than 85% of cases.1–5 The clinical characteristics of this manifestation do not differ much from those of many other respiratory diseases. It usually occurs with cough, fever, and an increase in usual dyspnea. It is not associated with any specific functional alteration, but a low diffusing capacity (as in our patient) or even positivity in a methacholine challenge test may be observed.1,3–6 The images obtained on chest X-ray are not usually pathological, but tracheal wall thickening may be seen on chest CT. Fiberoptic bronchoscopy often reveals diffuse edema of the tracheal mucosa and main bronchi, normally concurrently with whitish granular lesions with no clear distribution. In Crohn’s disease, biopsies tend to show non-specific chronic inflammatory infiltration with a predominance of neutrophils,7 while lymphocytosis is more predominant in other types of pulmonary manifestations of inflammatory bowel diseases.1–3
Evidence with respect to treatment is scant, and only clinical case series have been published. In most patients, this manifestation resolves with the administration of inhaled corticosteroids, which moreover help to prevent permanent lung damage.8,9 However, the administration of systemic corticosteroids or even immunosuppressants has been necessary in some series.10 Treatment with glucocorticoids is unsuccessful in approximately one third of patients with pulmonary manifestations, and immunosuppressive therapy may be required. A good option for immunosuppression may be azathioprine: Kar & Thomas reported good results7 with that approach, although their patient, unlike ours, presented ulcerative colitis. Infliximab has also been shown to greatly improve symptoms of patients with inflammatory bowel disease, and plays a significant role in the control of both gastrointestinal and pulmonary manifestations, as reported by Hayek.10 Treatment duration has not been established and varies greatly: from 2 weeks in the shortest schedules, up to 3 months in the longest. In our case, treatment continued at full dose for 1 month, and was then tapered over the following 2 months until discontinuation.
The mechanism of how inflammatory bowel disease can lead to pulmonary manifestations is still unknown. In embryonic development, the formation of the gastrointestinal tract and respiratory system originate in the same part of the embryonic structure and have a similar epithelial structure, so this might explain why the lung may become involved in this entity. However, many other alternative mechanisms have been proposed, such as bacterial dysbiosis, environmental pollution, or even genetic factors.1 For this reason, when performing a differential diagnosis in any patient with inflammatory bowel disease, the presence of manifestations of their underlying disease should be taken into account, especially in patients with cough and fever and no obvious infection. Although the incidence of these manifestations is still believed to be low, underdiagnosis seems likely, given the similarity of diagnostic test results and the fact that many patients who respond well to inhaled corticosteroids may be classified as asthmatics.6,7 We must, therefore, take into account this diagnostic possibility when we encounter patients with these characteristics.
Please cite this article as: Lojo-Rodríguez I, et al. Afectación traqueobronquial por enfermedad de Crohn. Arch Bronconeumol. 2020;56:122–124.