Mucosal associated lymphoid tissue (MALT) lymphomas are B-cell non-Hodgkin lymphomas that appear in extranodal sites, usually with no organized lymphoid tissue. The organ most frequently involved is the stomach, but there are reports of MALT lymphomas appearing in other locations in the digestive tract, lungs, skin, thyroid gland and orbit.1
Non-gastric MALT lymphomas typically have an indolent course, and are usually localized at diagnosis,2 with favorable prognosis3 and prolonged survival.1
Tracheal MALT lymphomas are exceedingly rare, regardless of primary or secondary involvement,3 probably due to the paucity of lymphoid tissue in this location.2 This type of MALT lymphoma appears to have similar characteristics to other non-gastric lymphomas, considering the response to treatment, prognosis and survival.
We report the case of an 86-year-old male who presented with a 1-week history of moderate hemoptysis and a 1-month history non-quantifiable weight loss. He had been previously treated with azithromycin for 5 days, 500mg/day, without results.
The patient was a non-smoker, on chronic antiplatelet therapy, with history of temporal arteritis, arterial hypertension, and non-Hodgkin MALT lymphoma of the right orbit diagnosed in July 2013, Ann Harbor IEA stage. He underwent chemotherapy with chlorambucil and prednisolone (8 cycles) and local radiotherapy (40Gy), finishing treatment in May 2014 with residual mass. Although radiotherapy is the recommended treatment in this stage, chemotherapy is also considered effective in all stages of MALT lymphoma.4 In this particular case, since the patient was elderly and lived far from the hospital, the option requiring less dislocations was chosen. It was also decided that if he presented with non-responsive disease or incomplete response, he would then undergo local radiotherapy, which was in fact the case.
On admission, he had bibasal crackles on pulmonary auscultation, with no other significant findings in the physical exam. The nose and throat examination ruled out upper airway lesions and local invasion of the orbital lymphoma.
Laboratory data showed normal levels of hemoglobin, platelets and coagulation tests. The chest X-ray revealed loss of volume on the right lung, consistent with previous findings. Chest computed tomography (CT) angiography was performed revealing signs of sub-segmental pulmonary thromboembolism (PTE) and also a retro-tracheal lesion, with tracheal lumen invasion.
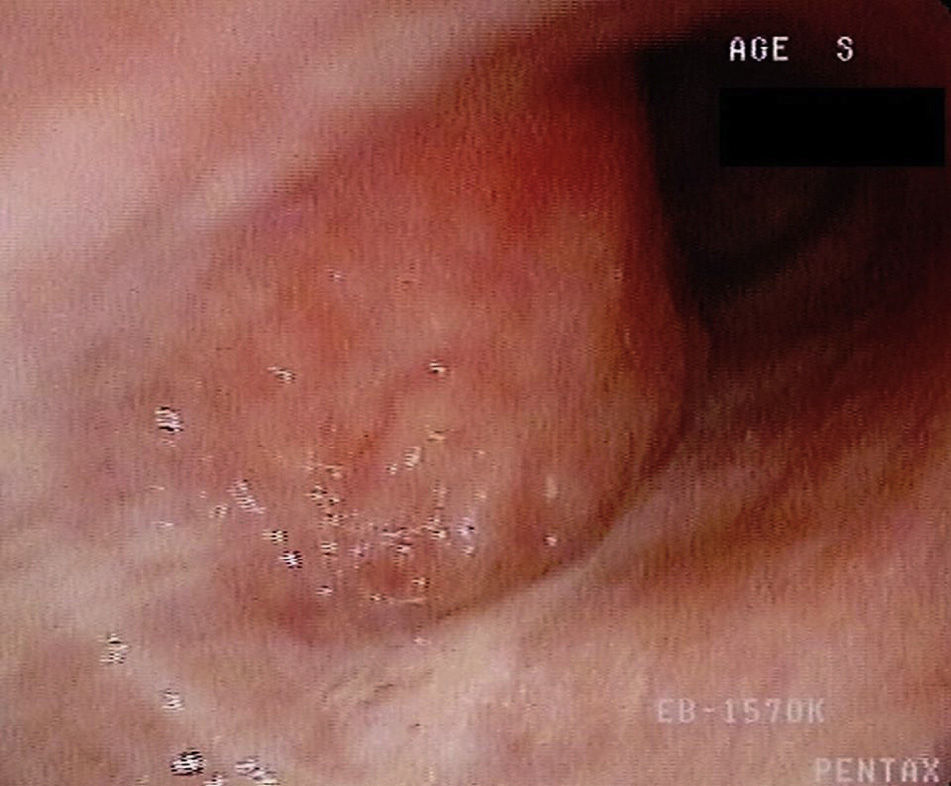
The patient underwent fiberoptic bronchoscopy that revealed a hypervascularized neoformative lesion of the posterior wall of the trachea that reduced tracheal diameter by 50% (Fig. 1). Biopsy histological analysis showed tracheal mucosal invasion by small lymphocytes with slightly irregular nucleus and the presence of lymphoepithelial lesions. The immunohistochemical study revealed staining for CD20 and bcl-2 and absence of staining for CD3, CD5, CD10 and cyclin-D1, compatible with involvement of the tracheal mucosa by low grade MALT lymphoma.
Ventilation/perfusion scintigraphy was also performed, showing intermediate probability of PTE.
Antiplatelet therapy was discontinued, and the patient was treated with aminocaproic acid, prophylactic antibiotherapy with amoxicillin and clavulanic acid and anticoagulant doses of low molecular weight heparin. He was discharged on remission of hemoptysis.
As this was an elderly patient with relapsed and disseminated disease, the chosen treatment was chemotherapy with chlorambucil and prednisolone, and local therapy (with bronchoscopy or radiotherapy) if he didn’t respond. He has so far completed 8 cycles of chemotherapy and remains asymptomatic. Follow-up chest CT showed complete resolution of the tracheal mass.
Although tracheal MALT lymphoma is extremely rare, it is associated with favorable prognosis and long term survival. Several different therapeutic options have been shown to be effective in this disease (surgical resection, radiotherapy, bronchoscopic therapy, chemotherapy, immunotherapy (rituximab) and immunochemotherapy). Given its rarity, there is insufficient data to compare the different options available.
In the case of disseminated disease, the treatment guidelines for non-gastric lymphoma recommend chemotherapy alone or in combination with immunotherapy. Local radiotherapy should be used only in localized stages or in palliation of local symptomatic disease.4,5
Given the prognosis and survival of this disease, this is an important differential diagnosis in tracheal lesions.2,3 According to the Pubmed database, 20 cases have been reported worldwide; this is the first case described in Portugal.
Dr. Fortunato Vieira, Dr.ª Ana Loureiro, Dr.ª Marisol Guerra and Dr.ª Margarida Inácio.
Please cite this article as: Raimundo S, Alexandre A, Pinto C. Linfoma de tejido linfoide asociado con mucosas con afectación traqueal secundaria: un diagnóstico infrecuente. Arch Bronconeumol. 2016;52:567–568.