To the Editor,
We report the case of a 75-year-old man with no significant medical history who presented with progressive dyspnea even on minimal exertion, some weeks after surgery for arthrodesis of the dorsolumbar spine.
On admission, elevation of the right hemidiaphragm was observed that was not present on previous radiographs, along with severe respiratory failure (pO2 49, pCO2 41) that showed little improvement after the administration of high-flow oxygen therapy, maintaining SpO2 of 90%–91% with a face mask with reservoir bag. When the patient stood up, he developed tachypnea and SpO2 fell to 84%–85%.
No signs of heart failure or respiratory failure were observed and right-sided paralysis of the diaphragm was confirmed with ultrasonography. Baseline laboratory tests were normal and a chest computed tomography with contrast ruled out pulmonary thromboembolism and parenchymal involvement, but revealed significant compression of the right atrium (RA) and partial atelectasis of the lower lobe of the right lung caused by the ipsilateral hemidiaphragm (Fig. 1A). Respiratory function tests showed a mild-moderate ventilatory limitation (FVC 76%, FEV1 64%, FEV1/FVC 65%), without impairment of CO diffusion capacity.
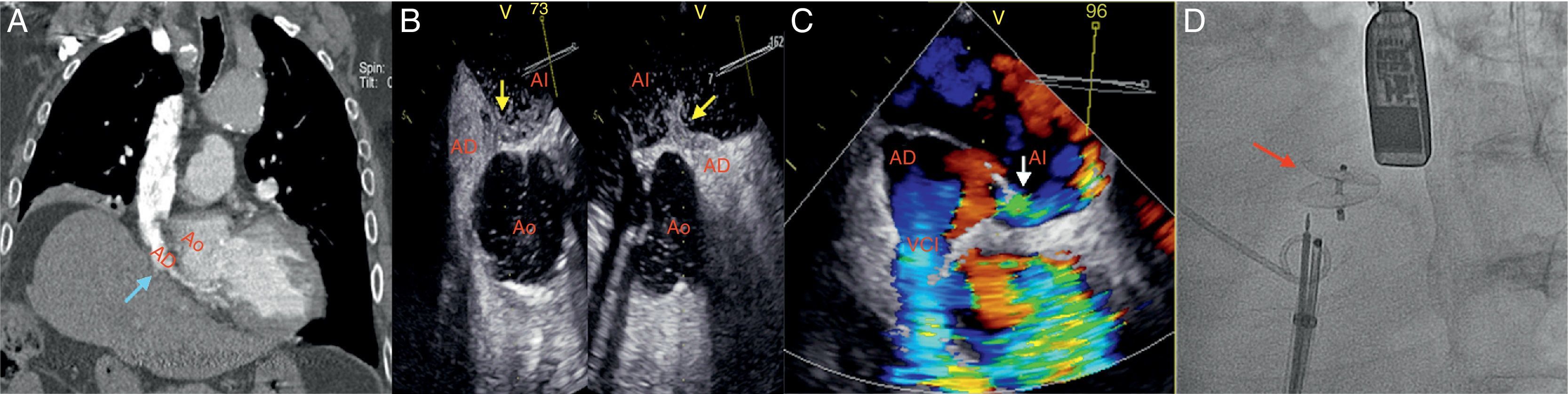
(A) Chest computed tomography with contrast medium: right atrial compression due to elevation of the ipsilateral hemidiaphragm (blue arrow). (B and C) Transesophageal echocardiogram: right-to-left shunt through the foramen ovale (passage of contrast medium to the left atrium – yellow arrow; color-Doppler – white arrow). (D) Amplatzer® device (red arrow).
AD: right atrium; AI: left atrium; Ao: ascending aorta; VCI: inferior vena cava.
The absence of lung disease that would explain the severe hypoxemia, and the poor response to oxygen therapy led us to suspect a pulmonary or right-to-left cardiac shunt. Transthoracic echocardiogram revealed the immediate passage of bubbles to the left cavities through the interatrial septum after intravenous administration of agitated saline contrast, suggesting a probable patent foramen ovale (PFO). The heart chambers were not dilated and pulmonary pressures were normal. A transesophageal study was performed, showing an RA severely reduced by extrinsic compression, confirming the presence of a right-to-left shunt via a PFO (Fig. 1B and C).
Given the patient's respiratory failure and symptoms consistent with platypnea-orthodeoxia syndrome, percutaneous closure of the PFO was indicated. A no. 18 Amplatzer® PFO occluder (St Jude Medical, USA) was implanted under transesophageal echography guidance (Fig. 1D), with minimal persisting residual shunt. After the procedure the patient's clinical situation and blood gases improved significantly, with stable SpO2>94% on room air at the time of discharge.
Persistent PFO is very common in adults, although a large majority of cases are silent.1 The development of symptoms is associated with increased pressure in the RA above the left atriums, leading to right-to-left shunt that can present clinically with embolisms, including cryptogenic stroke, or as varying degrees of hypoxemia.1 The shunt can increase in some circumstances, such as after interrupting Vlasalva maneuver, increased right ventricular afterload or changes in posture.1
The shunt can sometimes, though rarely, be caused by other anatomical factors, in the presence of normal right side pressures.2 Compression caused by an aneurysm or elongation of the thoracic aorta or by right diaphragmatic paralysis can modify the architecture of the RA and the morphology of the interatrial septum, directing the flow entering from the inferior vena cava directly toward the foramen ovale2,3 In our case, paralysis of the diaphragm produced a right-to-left shunt with normal pulmonary pressures.
Diaphragmatic paralysis is an uncommon clinical finding, sometimes associated with previous thoracic surgery, and can cause some degree of desaturation, and especially ventilation-perfusion mismatch due to loss of alveolar volume. Platypnea-orthodeoxia syndrome is an exceptionally unusual consequence.3,4 In the absence of significant pulmonary disease, non-hypercapnic respiratory failure refractory to oxygen therapy with an increased alveolar-arterial gradient, or worsening of symptoms when standing, should lead to suspect a possible intracardiac shunt.5 Although certain anatomical factors can contribute to hypoxemia, if PFO is found, percutaneous closure should be the treatment of choice.3
Please cite this article as: Benito-González T, Díez-Fernández F, Pérez de Prado A. Insuficiencia respiratoria asociada a parálisis diafragmática: ¿solo un problema de ventilación-perfusión?. Arch Bronconeumol. 2016;52:566–567.