We present the case of a 69-year-old patient, ex-smoker, diabetic and dyslipidemic, who was referred from another center with the diagnosis of pulmonary adenocarcinoma obtained with bronchoscopy that demonstrated a tumor in the orifice of the anterior segmental bronchus of the right upper lobe. Positron-emission tomography CT (PET-CT) confirmed a paramediastinal mass with increased uptake (SUVmax. 15g/ml) in the RUL compatible with a malignant tumor, right lower paratracheal lymphadenopathy with a fatty center with no FDG uptake and a right upper paratracheal lesion measuring 8mm, which was discretely hypermetabolic (Fig. 1A and B) and interpreted as a lymphadenopathy. Given these findings, the mass was staged as T3NxM0. As the patient was a candidate for radical surgical treatment, it was considered necessary to obtain samples in order to rule out N2 affectation.
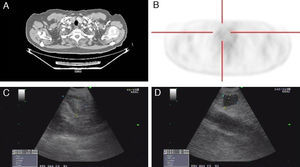
(A) Axial chest CT slice in the mediastinal window showing an upper right paratracheal nodule. (B) The cross-sectional PET-CT slice shows evidence of a right upper paratracheal lesion that is discretely hypermetabolic. (C) Ultrasound image of the lower right paratracheal lymphadenopathy, measuring 13mm×10mm, with a fatty center. (D) Subglottic hypoechogenic nodular image, measuring 8mm×7mm, corresponding with a thyroid cyst.
Sectorial endobronchial ultrasound (Olympus BF-UC 180F, Olympus, Tokyo, Japan) revealed a right lower paratracheal lymphadenopathy measuring 13mm×10mm with a fatty center (Fig. 1C) that was aspirated and resulted negative for malignant cells; in addition, there was a hypoechogenic nodule in the upper right paratracheal region (practically subglottic), measuring 8mm×7mm (Fig. 1D), which Doppler ruled out as a possible blood vessel. The ultrasound characteristics of said lesion were suggestive of a cyst, and needle aspiration obtained a liquid that the pathological analysis demonstrated to have follicular cells in plaques and groups, abundant macrophages and hemosiderophages on a background of colloid material, all of which were compatible with a thyroid cyst.
The existence of false positives from PET-CT in the mediastinal staging of lung cancer requires cytohistologic confirmation based on minimally invasive techniques such as ultrasound bronchoscopy. In this direction, recently published studies report a negative predictive value of PET-CT of 95%.1
Most thyroid nodules detected in patients with pulmonary neoplasm are usually benign lesions. Nonetheless, thyroid metastases in lung cancer have been described by some authors.2 It is for this reason that cytological confirmation is essential when given a patient with malignant lung disease.
Thyroid cysts are nodules with liquid content, located in the thyroid and differentiated from the rest of the parenchyma. Some papers have been published about the clinical implications and recommended management in neoplastic patients in whom uptake is detected by PET in the thyroid. The prevalence of this finding ranges between 1.2% and 4.3% of cases. The risk for malignancy of these lesions can reach 33%, corresponding with thyroid carcinomas (medullar or papillary), and in no case was it a metastasis of a primary neoplasm. In addition, the value of the SUVmax is not useful in order to differentiate between the benign or malignant nature of these lesions; therefore, cytohistologic confirmation is highly recommended.3,4
After reviewing the literature to date, we have only identified one single case published in a patient with small-cell lung cancer.5
We would like to emphasize the importance of confirming positive PET-CT findings in the mediastinum in patients with lung cancer, as well as the usefulness of sectorial endobronchial ultrasonography for the identification and complication-free needle-aspiration of thyroid cysts.
Please cite this article as: Sánchez-Font A, et al. Diagnóstico de quiste tiroideo mediante ultrasonografía endobronquial sectorial con punción-aspiración en un paciente con cáncer de pulmón. Arch Bronconeumol. 2012;49:38–9.