Thrombi in right cardiac cavities, described in less than 4% of patients with pulmonary embolism, are rare and in most cases confer a poor prognosis.1–3 Nevertheless, there is no consensus on the treatment of choice in these patients.
We report the case of a 72-year-old man, former smoker, diagnosed with severe COPD, Parkinson's disease and Pick's disease, who consulted the emergency department for a sudden onset of loss of strength and sensitivity in the right side of the face and right hand, along with dysarthria. The stroke code was activated, and a perfusion computed tomography (CT) was performed which revealed early signs of acute infarction in the left middle cerebral artery. Due to the low initial deficit and the progressive improvement of the clinical picture, fibrinolysis was rejected.
During his stay in the emergency department, the patient developed epigastric pain. An electrocardiogram was performed showing negative T waves in DI to DII, in aVF and V1–V6. Serial troponin T determinations rose from 38 to 570ng/L.
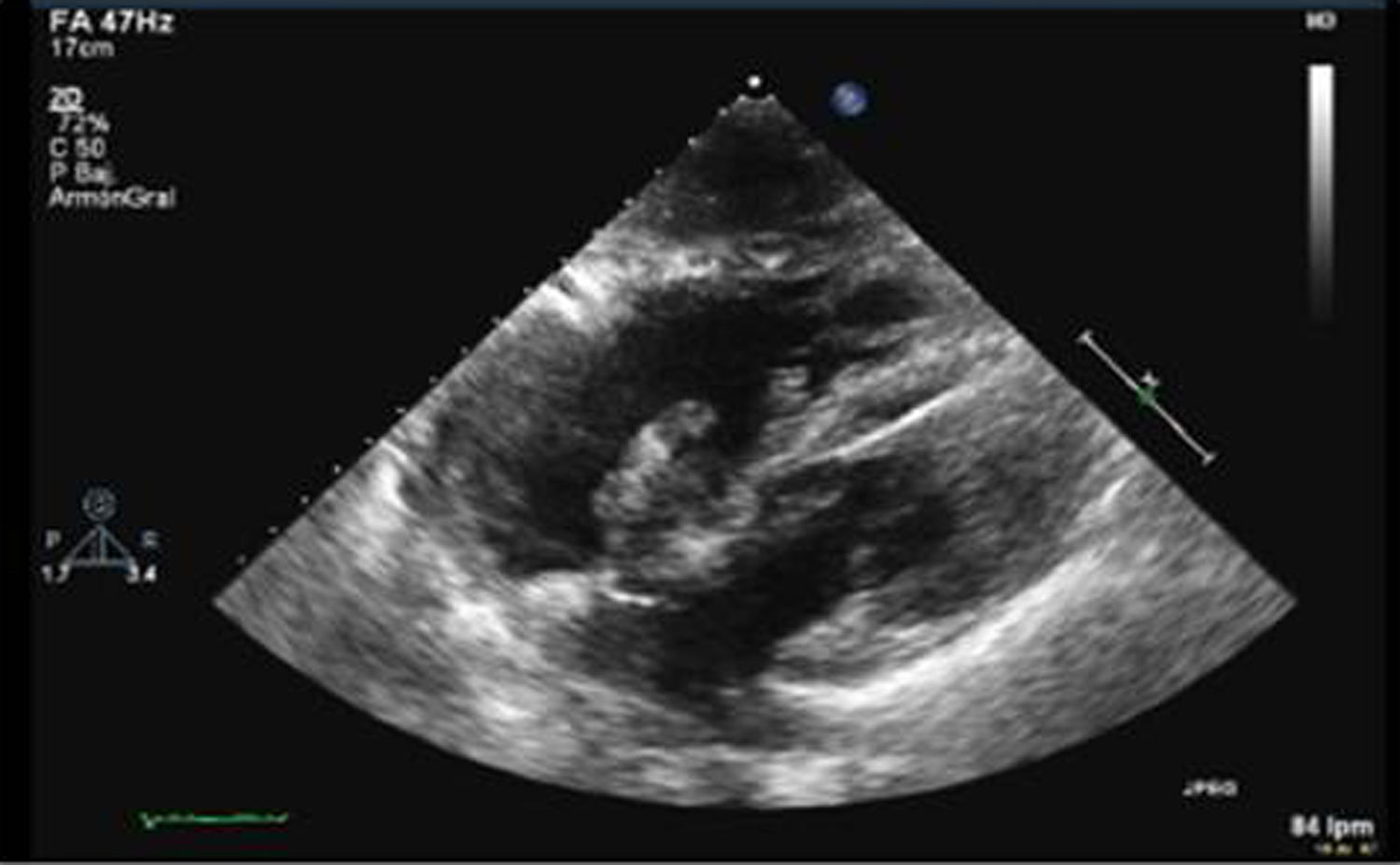
Acute coronary syndrome was suspected, so a transthoracic echocardiogram was performed, which revealed an image consistent with very long, mobile thrombi in both the left atrium and the right atrium each measuring approximately 4cm, that appeared to cross continuously through a patent foramen ovale, suggestive of thrombus in transit (Fig. 1). Findings consistent with severe pulmonary hypertension and severe right ventricular dilatation and dysfunction were also observed.
To confirm the presence of thrombus in transit, the study was completed with a transesophageal echocardiogram, and a chest CT was requested in which acute pulmonary thromboembolism (PTE) was identified with bilateral involvement from the main branches, along with data suggestive of pulmonary hypertension and right cavity overload.
Given these findings, the patient was admitted to an intensive care unit for monitoring and treatment, despite being hemodynamically stable since his admission to the emergency room. The cardiac surgery department of the reference center was contacted, and surgery was ruled out in view of the high surgical risk presented by the patient. Conservative treatment with low molecular weight heparin was adopted and the patient was subsequently transferred to the pulmonology department.
During his stay on the ward, the patient remained clinically and hemodynamically stable at all times. A follow-up echocardiogram showed a significant decrease in thrombus size and right cavity involvement, so he was discharged after a hospital stay of 16 days.
After 1 month of follow-up by the dedicated pulmonary circulation clinic, he showed good progress, and an echocardiogram confirmed the disappearance of the atrial thrombus and normalization of the morphology and function of the right cavities. Oral anticoagulation with vitamin K was initiated with good tolerance and regular follow-up was continued. One year after the episode, he was continuing to receive indefinite anticoagulation, free of complications and with recovery of his baseline situation.
The treatment of choice of right cavity thrombus is not well defined. Therapeutic alternatives include anticoagulation, catheter-guided or systemic thrombolysis, and surgical embolectomy.
The European Society of Cardiology suggests the use of thrombolytics in these patients.4 However, to date, no clinical trials have demonstrated the efficacy of this treatment, and the only scientific evidence that exists are clinical case series and meta-analyses of these series, and results of registries focused mainly on pulmonary embolism.
The first meta-analysis published by Kinney et al. in 1989, which included 199 patients with right-cavity thrombus, proposed anticoagulation as a first option, as they observed lower mortality in patients receiving anticoagulant therapy compared with those treated with thrombolysis and embolectomy (30% vs 38% vs 38%).5 However, in the same year, the European Cooperative Study led by the European Echocardiography Working Group was conducted in the same number of patients, and found that patients who received anticoagulation showed higher mortality in the short term than those treated with thrombolysis or embolectomy (64% vs 40% vs 27%), so the authors suggested surgery as a more effective treatment.6
Years later, Rose et al. positioned themselves in favor of thrombolytic treatment after a retrospective analysis of 177 patients between 1966 and 2000 in which they observed that both anticoagulation and embolectomy showed a worse prognosis.7 In 2003, Torbicki et al. reported on a small cohort of 42 patients from the International Cooperative Pulmonary Embolism Register (ICOOPER), in whom they found a similar therapeutic response among all therapeutic options, with a mortality rate of 23.5% in anticoagulated patients, 20.8% in thrombolysed patients, and 25% in surgically operated patients.8 Subsequently, in 2015, a study by Athappan et al. was published, which also favored thrombolysis due to the increased survival compared to anticoagulation. However, there were no statistically significant differences between embolectomy and anticoagulant therapy.9
The management of the case discussed here was based on a recent study published in 2017 by Barrios et al., designed from the RIETE (Computerized Registry of Patients with Thromboembolic Disease), which included 325 patients with PTE and thrombi in the right cavities. There were no differences between reperfusion therapy and anticoagulation in terms of short-term survival and the presence of major bleeding. Reperfusion therapy was also associated with an increased risk of recurrence of venous thromboembolism. Therefore, they concluded that anticoagulation therapy was appropriate for most patients with co-existing PTE and right-cavity thrombus, and reperfusion therapy should be reserved for patients with PTE and shock or hypotension, regardless of the presence of thrombi in right cavities.10
However, in the light of the existing data, the debate on the treatment of choice of these patients remains open.
Conflict of InterestsThe authors state that they have no conflict of interests.
Please cite this article as: Chasco L, Ballaz A, Oribe MA, Artaraz A, Aramburu A, Velasco S, et al. Trombo en tránsito. Arch Bronconeumol. 2020;56:537–539.