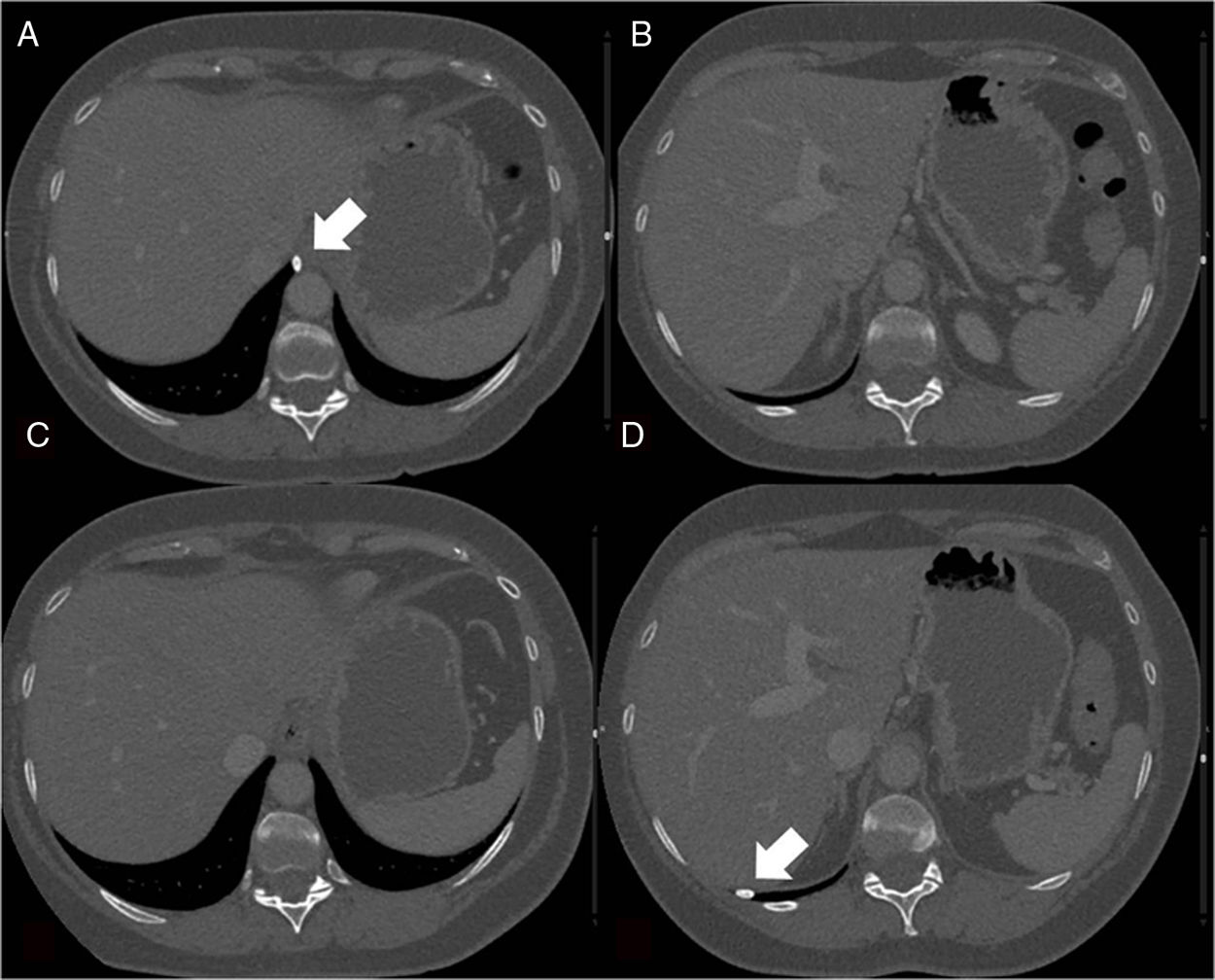
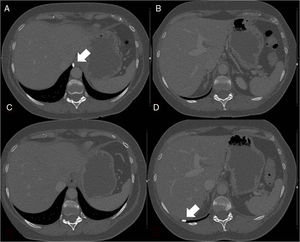
This was a 53-year-old female patient with a history of colon cancer diagnosed in 2016. A follow-up thoracoabdominal computed tomography (CT) revealed a calcified solid pleural nodule adjacent to the esophageal hiatus (Fig. 1A and B). A subsequent CT showed migration of the nodule within the pleural cavity to the posterior costophrenic recess, guiding a diagnosis of thoracolithiasis (Fig. 1C and D).
Thoracolithiasis is a rare entity with a prevalence of 0.086%.1 It consists of thoracoliths, bodies that can be calcified or not, which move about freely inside the chest cavity, in the absence of a history of trauma, intervention, or pleuritis.2 It is usually found incidentally in asymptomatic patients older than 50 years of age, most often in the left hemithorax. Although they can be calcified, thoracoliths can be indistinguishable on CT from intrapulmonary nodules. They are difficult to aspirate percutaneously, so diagnosis is usually made when migration of the nodule is observed. There have been several theories about their origin, the most plausible being that they arise from the detachment of a focus of pericardial or pleural fat necrosis,3 which would explain their histological composition and typical location.2
Please cite this article as: Cornellas L, Soler-Perromat JC, Vollmer I. Pleurolito: una rara causa de lesión torácica migratoria. Arch Bronconeumol. 2019;55:535.