We report the case of a 55-year-old man diagnosed with squamous cell carcinoma in the right upper lobe, preoperative pathological stage T3N0M0,1 who underwent right intrapericardial pneumonectomy (residual tumor measuring 4mm on resection border), and was treated with adjuvant chemotherapy and radiation therapy. After 5 months, the patient was referred to our clinic again, complaining of cough with whitish expectoration. Flexible bronchoscopy (FB) findings, not visible in the preoperative bronchoscopy, are shown in Fig. 1. Biopsies were obtained using Radial Jaw™ 4 2mm endoscopic forceps (Boston Scientific®), which were consistent with lobular capillary hemangioma in the bronchial stump (LCH). FB was scheduled for close endoscopic follow-up, and the patient showed no signs of malignancy or recurrent lesions, and no changes were found in the mucosa samples obtained over the following 3 years.
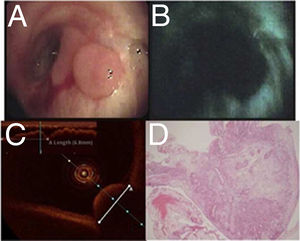
(A) Nodular lesion measuring 7.8mm in the post-pneumonectomy stump after visualization with conventional white light. (B) Endoscopic exploration with autofluorescence, with loss of the conventional appearance. (C) Optical coherence tomography showing an intact basal membrane. (D) Histological sample stained with hematoxylin eosin, 10× magnification, revealing the transition in the respiratory epithelium with a well delimited protuberance in the interior of the bronchial lumen with presence of angioblastic features and abundant leukocytes (polymorphonuclear subtypes), consistent with lobar capillary hemangioma.
LCH is a highly unusual acquired vascular lesion of non-neoplastic etiology that occurs in the lumen of the trachea, generally causing cough and hemoptysis.2 Despite the absence of a well-defined etiology, some of the hypotheses proposed suggest an association with minor trauma, endotracheal intubation, local irritation, bacterial and viral infections, or hormonal imbalances.3 To our knowledge, this is the first report of LCH described in a post-pneumonectomy stump.
Please cite this article as: de Vega Sánchez B, Disdier Vicente C, Borrego Pintado H. Hemangioma lobular capilar en muñón bronquial posneumonectomía. Arch Bronconeumol. 2019;55:536.