In the evaluation of a patient with pleural effusion (PE), clinical, radiological and pleural fluid data leads to the suspicion of malignancy.1–4 Following cytological analysis of the pleural fluid, chest computed tomography (CT) and other tests according to clinical criteria, a videothoracoscopy is indicated. This is the most efficient diagnostic method in malignant PE.5
Recent meta-analysis precludes routine recommendation of a positron emission Tomography (PET)-CT for discriminating malign from benign PE. PET-CT has proved useful in the study and staging of multiple neoplasms yet its role in patients with PE suspicious of malignancy has not been analysed.6
This is a prospective study to analyse the PET-CT in relation to thoracic CT of a consecutive series of patients with unclassified PE from October 2013 to June 2016. We included patients with unclassified effusions after clinical history, biochemical, microbiological and cytological analysis, without pleuropulmonary lesions in the chest-X-ray other than the PE, but in whom clinical suspicion of malignancy (defined by constitutional syndrome, high intensity asbestos-exposure, PE greater than 1/3 of the hemythorax or increasing at follow-up and bloody pleural fluid) was established and for whom thoracoscopy and pleural biopsy were indicated. Previously all patients underwent a thoracic CT and a PET-CT. All patients without diagnosis of malignancy (when malignant cells were detected in biopsy specimens.) were followed up until definite diagnosis was established or by means of clinical examination and imaging at 1, 3, 6 and every 6 months. The institutional ethics committee (CEIC PR(AG)149/2012) approved the study protocol, and the participants signed written informed consent.
Interpretation of chest CT imaging was done by a thoracic radiologist while interpretation of PET-CT imaging was carried out by a Nuclear Medicine Radiologist. They were blinded to the final diagnosis and both evaluated and registered a series of radiological findings and established a qualitative diagnosis of malignancy, benign or inconclusive.
The chi-square test (Fisher's exact test, when necessary) was employed to compare the clinical and radiological characteristics and the findings of the videothoracoscopy. To evaluate the association between the radiological findings from CT and PET-CT images and confirmed malignancy, a logistic regression was performed. Logistic regression was used to identify the best combination of CT and PET-CT findings to establish a better prediction of malignancy.
We included 42 patients with PE under study, 30 men and 12 women with a median age of 68 years old, for whom a diagnosis of malignancy had been established in 18, including 8 mesotheliomas (7 epithelioids and 1 sarcomatoid) and 10 metastasic (1 non-Hodgkin lymphoma, 1 adenocarcinoma of unknown origin and 8 NSCLC). Regarding the 24 benign effusions, 1 tuberculosis, 2 haemothorax and 1 LES were diagnosed.
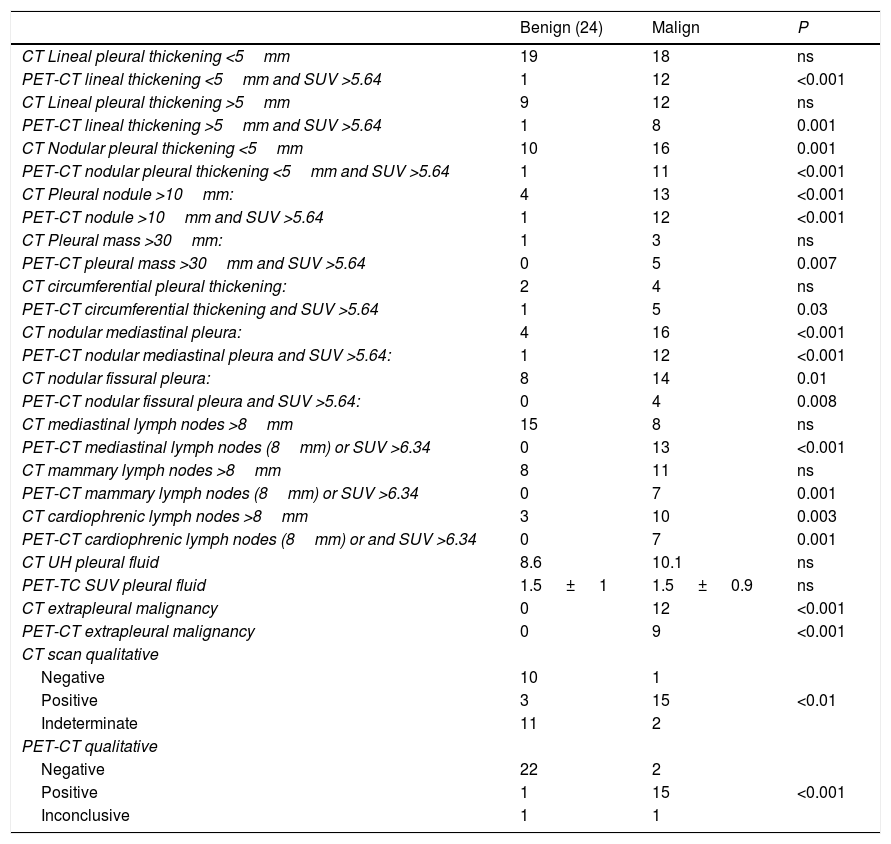
Regarding CT scan data, the univariate analysis is shown in Table 1. Logistic regression permits to establish a diagnosis in 85.4% of patients due to the combination of nodular pleural thickening below or above 5mm, the involvement of the mediastinal pleural node and adenopathy in the cardiophrenic angle, permitting correct diagnosis of 15 of the 18 malignant and 21 of the 24 benign effusions, with a sensitivity of 83%, specificity of 88%, VPP of 83% and VPN of 88% in the diagnosis of malignancy.
CT scan data and PET-TC data according to the definitive diagnosis of the patients.
| Benign (24) | Malign | P | |
|---|---|---|---|
| CT Lineal pleural thickening <5mm | 19 | 18 | ns |
| PET-CT lineal thickening <5mm and SUV >5.64 | 1 | 12 | <0.001 |
| CT Lineal pleural thickening >5mm | 9 | 12 | ns |
| PET-CT lineal thickening >5mm and SUV >5.64 | 1 | 8 | 0.001 |
| CT Nodular pleural thickening <5mm | 10 | 16 | 0.001 |
| PET-CT nodular pleural thickening <5mm and SUV >5.64 | 1 | 11 | <0.001 |
| CT Pleural nodule >10mm: | 4 | 13 | <0.001 |
| PET-CT nodule >10mm and SUV >5.64 | 1 | 12 | <0.001 |
| CT Pleural mass >30mm: | 1 | 3 | ns |
| PET-CT pleural mass >30mm and SUV >5.64 | 0 | 5 | 0.007 |
| CT circumferential pleural thickening: | 2 | 4 | ns |
| PET-CT circumferential thickening and SUV >5.64 | 1 | 5 | 0.03 |
| CT nodular mediastinal pleura: | 4 | 16 | <0.001 |
| PET-CT nodular mediastinal pleura and SUV >5.64: | 1 | 12 | <0.001 |
| CT nodular fissural pleura: | 8 | 14 | 0.01 |
| PET-CT nodular fissural pleura and SUV >5.64: | 0 | 4 | 0.008 |
| CT mediastinal lymph nodes >8mm | 15 | 8 | ns |
| PET-CT mediastinal lymph nodes (8mm) or SUV >6.34 | 0 | 13 | <0.001 |
| CT mammary lymph nodes >8mm | 8 | 11 | ns |
| PET-CT mammary lymph nodes (8mm) or SUV >6.34 | 0 | 7 | 0.001 |
| CT cardiophrenic lymph nodes >8mm | 3 | 10 | 0.003 |
| PET-CT cardiophrenic lymph nodes (8mm) or and SUV >6.34 | 0 | 7 | 0.001 |
| CT UH pleural fluid | 8.6 | 10.1 | ns |
| PET-TC SUV pleural fluid | 1.5 ± 1 | 1.5 ± 0.9 | ns |
| CT extrapleural malignancy | 0 | 12 | <0.001 |
| PET-CT extrapleural malignancy | 0 | 9 | <0.001 |
| CT scan qualitative | |||
| Negative | 10 | 1 | |
| Positive | 3 | 15 | <0.01 |
| Indeterminate | 11 | 2 | |
| PET-CT qualitative | |||
| Negative | 22 | 2 | |
| Positive | 1 | 15 | <0.001 |
| Inconclusive | 1 | 1 | |
Regarding PET-TC data, the univariate analysis is shown in Table 1. Logistic regression permits to establish a diagnosis in 95.2% of the patients due to the combination of any pleural thickening with SUV level greater than 5.64 and the presence of mammary adenopathy with SUV level above 6.34, which allows a diagnosis to be established for 16 of the 18 malign and the 24 benign effusions with a sensitivity of 89%, specificity of 100%, VPP of 100% and VPN of 92% for diagnosis of malignancy.
In 3 patients with initial anatomopathalogical study negative a neoplasm was observed in the follow-up. One of the patients with suspicion of malignancy using chest CT and PET-CT repeated pleural biopsy provided a diagnosis of mesothelioma, and has therefore been included in the malignant group for sample analysis. Another patient with chest CT and PET-CT not suggestive of malignancy and with a negative thoracoscopy on two occasions, died of pneumonia during follow-up. The autopsy showed pleural sarcomatoid mesothelioma 2.1×2cm stage T1aN0M0 and included in the malignant group. At two year follow-up another patient presented contralateral lung neoplasm with PE which was not related to the undiagnosed effusion.
Following analysis of the pleural fluid, thoracic CT is often the first diagnostic test performed.7,8 However, although a chest CT does not inform malignancy, as 35% of patients will have neoplastic PE.8 Recent meta-analysis also showed moderate accuracy of PET-TC for discriminating malign from benign PE.6
Classically, CT findings described as being suggestive of malignancy were nodular thickening or thickening greater than 1cm, thickening of the mediastinal pleura and circumferential thickening.9,10 In our patients both nodular pleural thickening and fissural or mediastinal nodular involvement show significant differences, as to do the cardiophrenic lymph nodes and evidence of extrapleural malignancy and has permitted correct classification of 85.4% of patients with correct diagnosis established for 21 of the 24 benign and 15 of the 18 malignant effusions.
The PET-CT study, allows the identification, location and quantification through the SUV.6 Multiple regression analysis permits correct diagnosis to be established in 95.2% of the patients due to the combination of any pleural thickening with SUV level greater than 5.64 and the existence of mammary adenopathy with SUV above 6.34, which means correct diagnosis of all the benign effusions and 16 of the 18 malign effusions.
Thus, although recent meta-analysis concluded that there is no data which justify its performance, PET-CT was not analysed in the group of patients with suspicion of malignancy .6
While we are aware that a small number of patients were analysed in this study and that therefore, further prospective studies evaluating the role of the PET-CT are needed, we believe our results suggest the PET-CT may play an important role in the study of undiagnosed patients.