Foreign body (FB) aspiration is a common problem in children and adults, necessitating prompt recognition and early treatment to minimize the potentially serious and sometimes fatal consequences.1,2 Consequences of an aspirated FB include the possibility of complete or partial airway obstruction, post-obstructive pneumonia, respiratory distress, pneumothorax or hemorrhage. Risk factors for FB aspiration include intellectual disability, neuromuscular diseases, maxillofacial trauma, unconsciousness, intoxication, dementia, and use of sedative drugs and dental medications.3
At present, FB removal in adults relies mainly on bronchoscopic techniques, including rigid and flexible bronchoscopy. A rigid bronchoscope provides greater access to the subglottic airways, ensuring correct oxygenation and easy passage of the telescope and grasping forceps during the extraction of a large FB. Furthermore, a rigid bronchoscope allows efficient airway suctioning if a massive bleed occurs.2,4 Flexible bronchoscopy offers several advantages compared with rigid bronchoscopy: first, it is more cost effective and easily applicable in an outpatient setting. Second, it avoids the need for anesthesia and deep sedation. Finally, it has been shown to be associated with lower mortality compared with rigid bronchoscopy (1% vs 12%), a difference which may be attributable to the avoidance of general anesthesia.5,6
It is difficult to extract large FBs from the airway using a flexible bronchoscope, especially FBs such as dental prostheses. The irregular surface and hard composition of dental prostheses make them particularly difficult to grasp and extract using normally effective instruments (e.g. biopsy forceps, Fogarty balloon catheters, alligator forceps, or wire baskets). For this reason, practitioners commonly use a multidisciplinary approach or a combination of instruments. In this case report, we describe the successful removal of a very large dental prosthesis that nearly totally occluded the right main bronchus of a 72-year-old woman following a myocardial infarction.
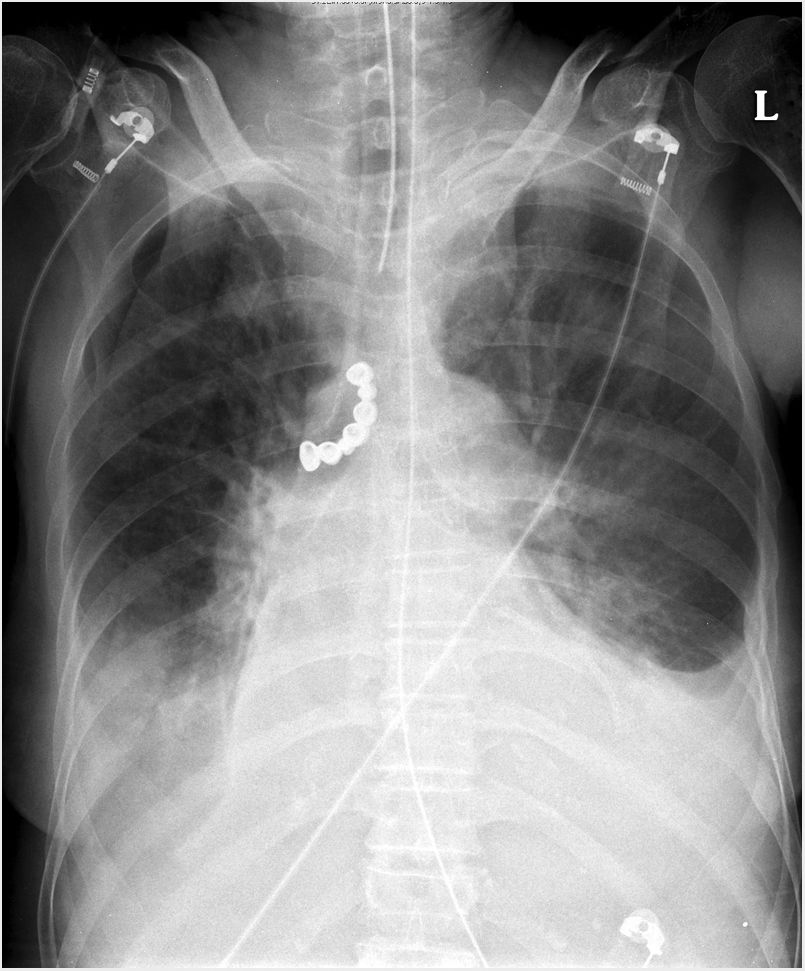
A 72-year-old female patient was admitted to the hospital due to an anterior wall ST elevation myocardial infarction. She underwent a primary percutaneous coronary intervention with the insertion of a stent to her left anterior descending coronary artery. She was intubated due to severe pulmonary edema and then safely weaned from mechanical ventilation seven days later. Ten hours after extubation, the patient suddenly developed dyspnea, tachypnea and severe hypoxemia. On physical examination, there were no signs of pulmonary edema, though decreased breathing sounds were noted on her right hemithorax. She underwent an immediate re-intubation, and an emergent chest X-ray revealed a large, fixed 7-unit restoration dental prosthesis nearly totally occluding the right main bronchus (Fig. 1).
Since the prosthesis was much wider than the 7.5-mm diameter of the endotracheal tube, we needed an innovative strategy for its extraction to avoid tracheotomy. A flexible bronchoscope was inserted through the endotracheal tube, after which the prosthesis could be seen in the right main bronchus. After a few attempts, the slippery prosthesis was finally grasped by large alligator forceps and the process of slowly withdrawing the scope began. When the prosthesis reached the distal end of the endotracheal tube, the complex of the tube, the bronchoscope and the grasped prosthesis were withdrawn until the prosthesis was brought to the level of the oropharynx. The prosthesis was extracted using Magill forceps together with the tube and bronchoscope. Immediately following the extraction, a new endotracheal tube was inserted. The patient tolerated this procedure well; she was weaned from mechanical ventilation the following day and discharged from the hospital 10 days later.
Foreign body (FB) aspiration is a common problem necessitating prompt recognition and early treatment to minimize the potentially serious and sometimes fatal consequences.1 Aspiration of a very large FB can constitute a technical problem, since its extraction may require an invasive procedure, such as rigid bronchoscopy, tracheotomy or thoracotomy, especially in an intubated patient. The use of a flexible bronchoscope decreases the risks associated with those procedures5,6 and has a high success rate (89.6%) in the extraction of FBs; thus, it should normally be considered as the initial approach. There are certain situations, however, in which a rigid bronchoscope should be considered, for example, with FBs that are impacted in extensive granulation tissue or excessive tissue scarring, asphyxiating FBs, FBs that cannot be gripped with flexible forceps as a consequence of their large size, sharpness and smooth margins, as well as failed attempts with a flexible one. In these cases, rigid bronchoscopy remains the procedure of choice.6 Nevertheless, in our case due to the patient's condition, and even though the FB was very large, we decided to begin immediately with a flexible bronchoscope.
Bronchoscopic procedures are not commonly performed in unstable patients, especially immediately following myocardial infarction, as it can result in fatal consequences. Pre-procedural planning is required and should include the whole care team: the bronchoscopist, assistants, nurses and anesthesiologist. Planning should involve discussion of the FB's characteristics, location, and the patient's comorbidities. Proper ventilation must be arranged for during the procedure, and a back-up plan developed to account for the potential that the foreign body may become lodged within the retro pharynx and completely occlude the airway.2 This scenario is more common when the FB is very large. In this case, the FB was indeed very large; however, the patient was also unstable, and so the normal pre-planning process was impossible and immediate action was required.
We describe the technique we used to successfully remove a large dental prosthesis in a mechanically ventilated patient, by extracting the FB with the endotracheal tube followed by an immediate re-intubation. Case reports on extractions of very large FBs are scarce. Sampan-Singh et al.,7 described extraction of a 3-unit dental prosthesis via direct laryngoscopy and tracheotomy. Tu et al.,8 described an approach using wire loop snares together with a flexible bronchoscope for the removal of a 4-unit dental prosthesis. Our patient aspirated a 7-unit dental prosthesis, which we believe represents the largest reported FB extraction by flexible bronchoscopy.
This case represents an emergent exceptional approach of extracting large foreign bodies from the tracheobronchial tree in an unstable patient, with relatively minimal temporary compromise of the airway, using only a flexible bronchoscope. The advantages of flexible over rigid bronchoscopes have been described; they provide applicable, cost-effective, safer and faster method of extraction of FBs, and thus should be considered first in experienced hands, even in cases in which rigid bronchoscopy is apparently indicated. Although reports on FB extraction are common, our case, which describes the removal of a very large prosthesis from the bronchial tree in a high-risk patient, is unique.