The objective of this study is to analyze the clinical characteristics of two COPD patient populations: one diagnosed using the lower limit of normal (LLN) and another diagnosed by the GOLD criteria. We also compared the population excluded by the LLN criterion with a non-COPD control population.
The COPD patients determined with the LLN criterion presented significantly lower levels of FEV1/FVC at 0.55 (0.8) vs 0.66 (0.2), P=.000; FEV1 44.9% (14) vs 53.8% (13), P=.000, and FVC 64.7% (17) vs 70.4%, P=.04. The two COPD groups presented more frequent ER visits in the last year (57% and 52% of the patients, respectively, compared with 11.9% of the control group), without any statistically significant differences between the two. This same pattern was observed in the number of ER visits in the last year: 1.98 (1.6), 1.84 (1.5), and 1.18 (0.7), respectively.
When we analyzed the prevalence of the comorbidities that are most frequently associated COPD, there was a clear increase in the percentage of patients who presented associated disorders compared with the control group. Nevertheless, these differences were not very relevant between the two COPD groups. The differences also were not relevant between both COPD groups in the pharmacological prescription profile.
In conclusion, the use of the LLN as a criterion for establishing the diagnosis of COPD, compared with the GOLD criteria, excludes a population with important clinical manifestations and with a high consumption of health-care resources. Before its implementation, the relevance of applying this criterion in clinical practice should be analyzed.
El objetivo de este estudio es analizar las características clínicas de 2 poblaciones de pacientes con EPOC, una diagnosticada utilizando el límite inferior de la normalidad (LIN) y otra por criterio GOLD, y comparar la población excluida por el criterio LIN con una población control sin EPOC.
Los pacientes con EPOC por criterio LIN presentaban valores significativamente más bajos de FEV1/FVC 0,55 (0,8) vs 0,66 (0,2), p=0,000; de FEV1 44,9% (14) vs 53,8% (13), p=0,000, y de FVC 64,7% (17) vs 70,4%, p=0,04. Los 2 grupos de EPOC presentaron una mayor frecuentación en urgencias en el último año (57 y 52% de los pacientes, respectivamente, frente al 11,9% del grupo control), sin que hubiera diferencias estadísticamente significativas entre ambos. Este mismo patrón se observó en el número de visitas a urgencias en el último año: 1,98 (1,6), 1,84 (1,5) y 1,18 (0,7), respectivamente.
Cuando se analizó la prevalencia de las comorbilidades que más frecuentemente se asocian a EPOC se detectó, frente al grupo control, un claro incremento en el porcentaje de pacientes que presentaban trastornos asociados; sin embargo, estas diferencias fueron poco relevantes entre los dos grupos de EPOC. Las diferencias tampoco fueron relevantes entre ambos grupos de EPOC en el perfil de prescripción farmacológica.
Como conclusión, el uso del LIN como criterio para establecer el diagnóstico de EPOC, frente al criterio GOLD, excluye una población con importantes manifestaciones clínicas y con un elevado consumo de recursos sanitarios. Antes de su implementación debe analizarse la relevancia de aplicar este criterio en la práctica clínica.
The SEPAR-ALAT guidelines define chronic obstructive pulmonary disease (COPD) as the presence of chronic airflow obstruction that is not reversible (reduction of forced expiratory volume in one second [FEV1] and the FEV1/forced vital capacity [FVC] ratio) mainly caused by an inflammatory reaction to tobacco smoke.1 This definition, which does not substantially vary from that proposed by GOLD2 or by the ATS-ERS,3 poses operative problems that limit its usefulness in clinical practice as it is based on an arbitrary cut-point whose clinical relevance has not been properly evaluated. The main advantage of using such a simple criterion is that it can contribute to the diffused use of spirometry, especially in the primary care setting, and that it reduces the confusion of recent years for establishing the diagnosis of COPD, especially in the less severe forms.
Without a doubt, the use of an FEV1/FVC ratio less than 70% can reduce this discrepancy, but it is necessary to recognize its limitations as this cut-point varies with age and height. It may therefore incorrectly classify the presence of obstruction at extreme ages.
As in other diseases, the prevalence of COPD can be conditioned by the criterion that is used to establish its diagnosis. With the use of the fixed ratio, there may be a high number of COPD overdiagnoses in healthy subjects who are older or tall, and the opposite may be true in short young subjects.4,5 The risk for overdiagnosis is especially relevant in patients over the age of 70. In a study by Hardie et al.6 of healthy non-smoker seniors, it was demonstrated that 35% of subjects over the age of 70 presented an FEV1/FVC ratio of <70%; this prevalence reached 50% if they were over the age of 80. At the other extreme, young patients in whom early detection can be relevant could be considered normal using the GOLD criteria.
In order to avoid these limitations, some authors recommend the use of the lower limit of normal (LLN).7,8 This posture has been recently supported by the ATS/ERS guidelines for interpreting spirometry, which recommend the use of the LLN to diagnose obstruction.9 Although it is founded on statistically solid concepts, this cut-point originates in cross-sectional or database studies but, from a clinical standpoint, their clinical relevance has not been clearly established compared with the GOLD criteria. Without this information, it is essential to be aware of any discrepancies derived from using one or the other criterion, as this can condition important differences, both from a clinical as well as from an epidemiological perspective.
Based on a cohort of patients diagnosed with COPD by the GOLD criteria, we analyzed the characteristics of the patients diagnosed with COPD by the LLN criterion and compared the population excluded by this criterion with a non-COPD control group.
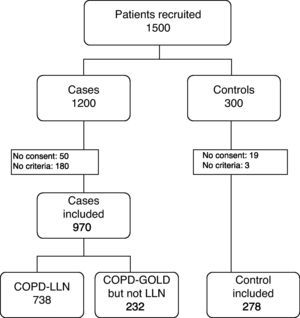
Materials and MethodsStudy Design and PopulationThe data for this study are those of the CONSISTE (Consecuencias Sistémicas de la EPOC–Systemic Consequences of COPD) project, which is a multi-center, cross-sectional study of cases and controls done at primary care consultations and specialized care consultations throughout Spain (Fig. 1). The prime objective of the project was to analyze the association between COPD and cardiovascular risk factors.
The inclusion criteria for the groups of cases were: age over 40, smoking history of more than 10 pack-years, COPD diagnosis defined by the presence of a post-bronchodilator FEV1/FVC ratio <70%, clinical stability in the 8 weeks prior and written informed consent for participation in the study. Patients with chronic respiratory diseases other than COPD were excluded.
The control group was also established at the outpatient consultations, and the inclusion criteria were: age over 40, smoking history of more than 10 pack-years, clinically stable condition and written informed consent for participation in the study. In this group, subjects with non-obstructive spirometries (FEV1/FVC≥70%) were included, and the same exclusion criteria were applied as for the cases.
In order to avoid selection bias, both the cases as well as the controls were consecutively collected by the physicians participating in the study, as long as they met all the inclusion and none of the exclusion criteria.
By protocol, all the patients had had a previous follow-up of more than one year. All the data related with the study had been therefore recorded in the medical files of the participating centers, although the information was confirmed when the patient was selected.
ProceduresAt the time of inclusion, all subjects (controls and cases) provided data for their medical histories by means of a specifically designed questionnaire, including age, sex, smoking, weight, height, associated cardiovascular risk factors, presence of associated chronic comorbidity and pharmacological treatments related with COPD and cardiovascular factors. Likewise, the number of exacerbations was recorded, as was the consumption of health-care resources as estimated by doctors’ appointments, visits to the ER and hospitalizations during the previous year. Lastly, all the subjects underwent post-bronchodilator spirometry in order to confirm that they met the established diagnostic criteria.
From the population that was diagnosed with COPD by means of the GOLD criteria, two groups were established according to whether they met the COPD criteria using the LLN of the ECSC.10
Ethical AspectsThe study was approved by the Ethics and Clinical Research Committee of the Hospital General Universitario Gregorio Marañón, and all the patients were informed of the study characteristics and objectives, giving their written informed consent for participation.
Statistical AnalysisGiven the main characteristics of the study, in order to calculate the sample size, we used as a main variable the association of cardiovascular disorders in COPD, using data from the literature and previous results from the ARCE observational study11 as a reference. The high number of patients in each group and the data from the literature enables us to suppose that the size of the population analyzed is large enough for the objective of the study.
The results of the continuous variables have been presented with their means and standard deviation. In the categorical variables, the results are expressed as frequencies and percentages. The Kolmogorov–Smirnov test was used to study the normality of the numerical variables.
In order to analyze the differences between the groups in the quantitative variables, the Student's t-test was used in the variables with normal distribution and the Mann–Whitney U was used if the distribution was not normal. For the comparison of the means of several groups, the ANOVA test was used with the Bonferroni correction. The association between qualitative variables was studied with Pearson's chi-squared or Fisher's exact test. The association between quantitative variables was studied with Pearson's correlation coefficient or Spearman's r coefficient depending on the normality of the data.
The statistical analysis was done with the SPSS version 18.0 software. Results with a P<.05 were considered statistically significant.
Results23.2% (232/970) of the “overdiagnosed” patients with the GOLD criterion compared with the LLN presented a profile similar to the COPD cases diagnosed by LLN for the number of exacerbations that required hospital care, pharmacological treatment and associated cardiovascular disorders.
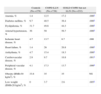
Table 1 presents the main characteristics of the 3 study populations. Out of the 970 patients selected, 1.35% were GOLD stage 1, 38.2% stage 2, 49.5% stage 3 and 11% stage 4. Only 738 (76%) of the subjects studied presented obstruction by the LLN criterion. When COPD was defined by the LLN criterion, patients were identified with a greater functional deterioration that the non-LLN GOLD population. The patients with COPD by the LLN criterion presented significantly lower FEV1/FVC values (0.55 [0.8] vs 0.66 [0.2], P=.000), FEV1% (44.9% [14] vs 53.8% [13], P=.0000) and FVC (64.7% [17] vs 70.4%, P=.04).
Characteristics of the Three Study Populations.
| Controls (No.=278) | COPD-LLN (No.=738) | GOLD COPD, but not LLN (No.=232) | ||
| Age, years | 59 (8) | 63 (8) | 66 (9) | 0 |
| Sex, males (%) | 74 | 67 | 84 | 0 |
| Pack-years | 34.5 (17.9) | 65.4 (34.6) | 66.9 (35.6) | .000a |
| BMI, kg/m2 | 28.7 (4.3) | 28 (6) | 27.9 (5.7) | NS |
| FEV1, % predicted | 97.1 (16) | 44.9 (14) | 53.8 (13) | 0 |
| FVC, % predicted | 97.5 (17) | 64.7 (17) | 70.4 (12) | 0 |
| FEV1/FVC | 78.9 (6) | 55.2 (8) | 66.5 (2) | 0 |
| Hemoglobin, g/dl | 15.2 (1.5) | 13 (2.9) | 13.2 (3) | .000a |
| CRP, mg/l | 2.6 (4.2) | 6.8 (3.9) | 7.2 (4.2) | 0 |
| ER visits in the last year, % patients | 11/09/12 | 57 | 52 | 0 |
| ER visits in the last year | 1.18 (0.7) | 1.98 (1.6) | 1.84 (1.5) | .02a |
| Hospitalizations in the last year, % patients | 06/05/12 | 36.2 | 32 | a |
| Hospitalizations due to COPD exacerbation, % patients | 0 | 32 | 28/09/12 | a |
| Number of hospitalizations due to COPD exacerbation | 0 | 1.1 (0.4) | 1.09 (0.4) | .000a |
BMI: body mass index; CRP: C-reactive protein; NS: not significant in the global analysis.
The 2 COPD groups presented a greater frequency in ER visits in the previous year (57% and 52% of the patients, respectively, compared with 11.9% of the control group), without there being any statistically significant differences between the two. This same pattern was observed in the number of visits to the ER in the last year: 1.98 (1.6), 1.84 (1.5) and 1.18 (0.7), respectively. Nor were there significant differences between the two groups of patients in the number of hospitalizations due to COPD: 1.1 (0.4) and 1.09 (0.49), respectively.
Table 2 demonstrates that when we analyze the prevalence of the comorbidities that are most frequently associated with COPD there is, compared with the control group, a clear increase in the percentage of patients with COPD who present associated disorders. These differences, however, were not very relevant between the two COPD groups and were only significant for ischemic heart disease.
Vascular Comorbidity in the Three Study Groups.
| Controls (No.=278) | COPD-LLN (No.=738) | GOLD COPD but not LLN (No.=232) | ||
| Anemia, % | 1.4 | 12.5 | 17.2 | .000a |
| Diabetes mellitus, % | 9.7 | 40.5 | 36.4 | .000a |
| Dyslipidemia, % | 31.7 | 49.6 | 44.3 | .000a |
| Arterial hypertension, % | 36 | 50 | 56.7 | .000a |
| Ischemic heart disease, % | 4.7 | 13.7 | 8.7 | .000 |
| Heart failure, % | 1.4 | 26 | 20.8 | .000a |
| Arrhythmia, % | 4.7 | 15.4 | 18.3 | .000a |
| Cerebrovascular disease, % | 2.9 | 9.7 | 10.8 | .001a |
| Peripheral vascular disease, % | 4.1 | 17.3 | 13.7 | .000a |
| Obesity (BMI>30kg/m2), % | 33.8 | 35 | 35 | NS |
| Low weight (BMI<20kg/m2), % | 0 | 3.7 | 2.6 | .005a |
BMI: body mass index; NS: not significant in the global analysis.
Table 3 presents the pharmacological prescription profile of the patients with LLN criterion and in the patients who were not classified as COPD by the LLN criterion. Short-acting bronchodilators were excluded as their occasional use is frequent in many intercurrent processes that cannot always be catalogued as COPD. The prescription profile is similar in both patient groups for the main bronchodilator and anti-inflammatory drugs.
Pharmacological Prescription in the Three Study Groups.
| Controls (No.=278) | COPD-LLN (No.=232) | GOLD COPD but not LLN (No.=738) | ||
| Ipratropium, % | 0 | 17.2 | 19.6 | NS |
| Tiotropium, % | 0 | 72.5 | 69.5 | NS |
| Inhaled corticosteroids with LABA, % | 0 | 54 | 53 | NS |
| Theophylline, % | 0 | 15 | 12 | NS |
| Mucolytic agents, % | 0 | 12 | 10.4 | NS |
| Statins, % | 20.5 | 22.1 | 18.5 | NS |
| ACE inhibitors, % | 11.2 | 27.7 | 24.9 | .000a |
| ARB II, % | 12.2 | 20.7 | 21.9 | .000a |
| Antiaggregants, % | 10.4 | 19.4 | 20.2 | .000a |
| Beta blockers, % | 11.2 | 5.1 | 6.5 | .000a |
| Calcium antagonists, % | 6.1 | 10.8 | 11.1 | .000a |
NS: not significant in the global analysis.
When we analyzed the consumption of drugs related with the treatment of the main cardiovascular disorders, the consumption of medication among COPD patients was clearly higher than in the control group, but with hardly any differences between both patient groups.
DiscussionThe main conclusion of this study is that, in standard clinical practice, the use of LLN for defining COPD excludes a large number of patients when compared with the GOLD criteria. This group of patients that was excluded by the LLN criterion presents important clinical manifestations and a high consumption of health-care resources, both in care provided as well as medication. These data suggest that before applying the LLN criterion, it is necessary to clarify which factors are implicated in the clinical deterioration of these patients, the reasons for why there is a high consumption of drugs related with COPD in a group that would not be identified as COPD when using the LLN criterion, and if the origin of its clinical deterioration is primarily pulmonary or whether it is associated with diseases apart from the pulmonary pathology.
In recent years, many initiatives have been aimed at obtaining a fast diagnosis and early treatment of COPD. Regarding the use of the FEV1/FVC ratio, its simplicity may favor its implementation in clinical practice and facilitate early diagnosis of the disease, although its clinical relevance has not been well established. This is especially true in GOLD stage 1, where there may be great discrepancies with other criteria based on statistical concepts such as the LLN. In an attempt at improving diagnostic precision, it has been proposed to use the FEV1/FVC ratio together with an FEV1 value below 80%, which would exclude GOLD stage 1. Nevertheless, this proposal is also not free from controversy, as even in this stage the presence of symptoms, reduced exercise capacity and increased mortality have been demonstrated.12–17 Furthermore, the greater or lower relevance of using this criterion could also be conditioned by age.8
Currently, there is a body of opinion that encourages the use of LLN for establishing the diagnosis of COPD. Supporting this posture, it has been reported that the ratio would incorrectly overdiagnose older patients as COPD. Another argument in favor of the use of LLN is that it would enable the disease to be detected early on in relatively young populations, which is where it is essential to introduce preventive measures to keep the disease from progressing further and to detect it in advanced phases. However, there are no studies that demonstrate that earlier detection in young subjects using LLN has a real impact in the disease evolution or load. Finally, to those who defend the use of FEV1/FVC over LLN based on its simplicity, an argument could be made that this aspect may be of little relevance because even the most basic current devices are able to incorporate the calculation of LLN, and the GOLD classification requires the use of theoretical values to establish severity levels.18
On the other hand, there are also arguments in favor of using the FEV1/FVC ratio because it is able to establish a limit of functional normality, regardless of the degenerative changes that occur with age, and thus this limit would be clinically transcendent, regardless of age.19 This standpoint assumes that the changes that occur with age do not necessarily reflect a situation of normality. This posture would be important if these changes required specific interventions, as in the case of the loss of eyesight. In practice, presbyopia could be considered normal in an age-adjusted statistical model; but, if a set limit of normality is used, it is possible to detect a problem and indicate a treatment, regardless of whether its presentation is practically universal as we age. However, in lung function these postures are theoretical and there are no consistent arguments that demonstrate their usefulness in clinical practice. For this reason, aside from theoretical considerations, the use of a certain criteria for establishing the diagnosis of COPD should be based on its clinical relevance and not on aspects of apparent simplicity, which may be easily resolved with current technology.
The results of this study do not establish which criteria is better, but they do clearly indicate that with the use of the LLN criterion there is a high percentage of patients who would be excluded from the diagnosis. These patients make up a population that has important clinical manifestations and a high consumption of health-care resources, with a clinical profile similar to other COPD patient groups that is very different from the control population. There are many possible factors that influence this situation, and they are not always related with airflow obstruction (associated diseases, weight problems, etc.) which should be specifically studied in this population type.20–23 Until we have this information, the patient should be assessed by the clinician, but the use of a criterion like LLN would exclude from the start an important population that, due to the consumption of health-care resources that it represents, requires proper medical evaluation.
It is also necessary to establish which criterion is best from an epidemiological standpoint.24 Aside from the marked discrepancies in the prevalence of the disease that there may be (depending on the criterion used) any analysis that tries to establish a relationship between COPD and other processes (e.g. vascular disease) should be based on a criterion that is not arbitrary. In our series, the use of LLN did not improve the results that had been previously obtained in the ARCE study.25 In that study, which included a smaller population and did not have a control group, the use of the LLN did not substantially modify the results obtained with GOLD when evaluating the association of COPD with vascular disorders. In this current study, using the LLN criterion, we have found a greater prevalence of ischemic heart disease in the COPD group, but there were no significant differences for other cardiovascular risk factors, cerebrovascular lesions or peripheral vascular lesions. The complexity of COPD, with different patient profiles for one same functional loss, complicates relationships of this kind, be it with either the GOLD or LLN criteria.
The main limitation of our paper was that it is a cross-sectional study, and the data should therefore be confirmed by longitudinal studies. Although such an approach would be ideal, it would entail a great delay, and while waiting for the results to be in possibly a high number of patients with important clinical affectation would be excluded from a proper assessment if the LLN criterion were used.26
Another limitation is that the population of this study was made up of patients seen in the pulmonology and primary care departments due to respiratory symptoms. Therefore, the results cannot necessarily be extrapolated to the general population. Nevertheless, in a population-based study, García-Rio et al.27 also observed no differences between the 2 groups for respiratory exacerbations, distanced walked in the 6-min walk test or in systemic biomarkers.
Last of all, it is possible that, by selecting the sample from patients with COPD diagnosis using the GOLD criteria, short young patients with mild COPD may have been excluded. This aspect may be relevant in early detection programs, but it is not very important in daily clinical practice. The mean ages of the COPD groups were 63 and 66, similar to the age reported in other series using the characteristics of patients with COPD seen in primary specialized care consultations.28
In conclusion, the use of LLN as a criterion for establishing COPD diagnosis, compared with the GOLD criterion, excludes a high number of patients with important symptoms and a high consumption of health-care resources. Before applying this concept in clinical practice, it is necessary to analyze in detail the population group that was excluded and to determine which factors are associated with the symptoms and the high consumption of health-care resources.
FundingThis study has been funded by Esteve Laboratories.
Members of the group CONSISTE: Juan José Soler, Aurelio Arnedillo, Adolfo Baloira, Rosa Güell, Jesús Molina and Karlos Naverán.
Please cite this article as: Izquierdo Alonso JL, et al. El uso del límite inferior de la normalidad como criterio de EPOC excluye pacientes con elevada morbilidad y alto consumo de recursos sanitarios. Arch Bronconeumol. 2012;48:223–8.