To quantify the degree of compliance with the recommendations of the clinical practice guidelines published in 2009 by the ERS and the ESTS regarding the preoperative assessment of risk of lung resection in daily clinical practice at a tertiary hospital.
MethodA prospective, observational study of real-time data collected from consecutive patients who had been referred for evaluation from September 2009 to December 2010. We recorded the presence or absence of the recommended studies included in the algorithm, their results and, when a test was missing, the reasons why it was not performed. Hospital mortality and cardio-respiratory morbidity rates are also presented.
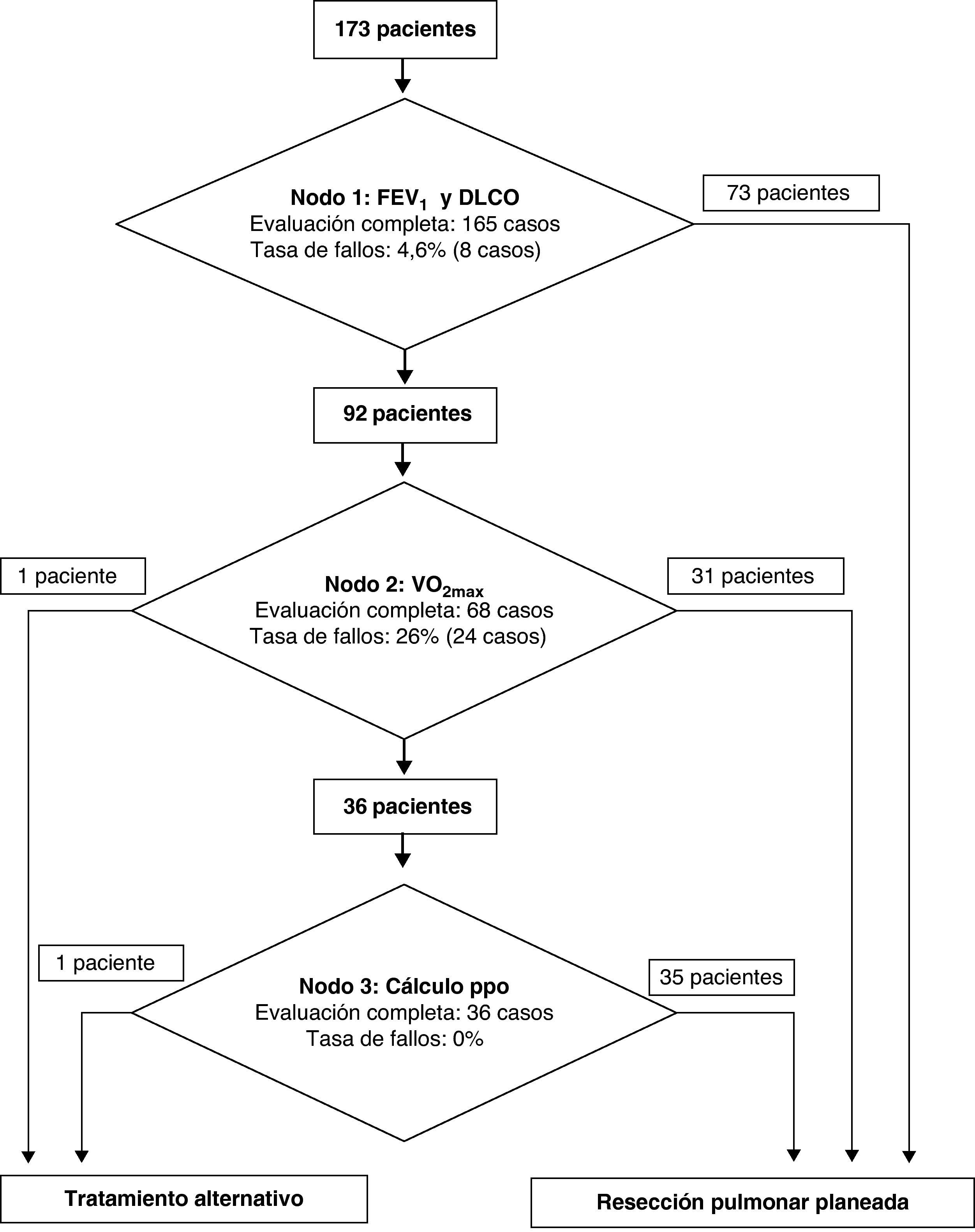
Results173 patients were evaluated. In 171 cases, lung resection was performed, with a mortality of 1.2% and a cardio-respiratory morbidity of 11.7%. The failure rate of the first level of the algorithm was 4.6% and for the second level (VO2max test) it was 26%. The absence of exercise tests was mainly due to hospital structural problems and the patients’ inability to perform it. Out of the patients who performed the exercise testing, 31 reached a VO2max of 20ml/kg-min or more and underwent surgery without calculation of FEV1ppo and DCLOppo; 35 patients required the calculation to determine their operability and in 2 cases the intervention was not recommended due to functional inoperability of the patient.
ConclusionsThe validation process found lack of compliance with the proposed algorithm in 18.5% of the cases basically due to the absence of the exercise tests. The rate of adherence to the algorithm recommendations should be improved before performing any other validation studies.
Cuantificar el grado de cumplimiento de las recomendaciones contenidas en la guía en la práctica clínica publicada en 2009 por la ERS y la ESTS sobre evaluación preoperatoria del riesgo de la resección pulmonar en la actividad asistencial diaria de un hospital terciario.
MétodoEstudio prospectivo observacional. Registro de datos en tiempo real de los pacientes consecutivos remitidos para evaluación desde septiembre de 2009 a diciembre de 2010. Se ha registrado la presencia o ausencia de los estudios incluidos en el algoritmo, sus resultados y, en caso de ausencia de alguna prueba, por qué no se realizó. Se aportan las tasas de mortalidad hospitalaria y de morbilidad cardiorrespiratoria postoperatoria.
ResultadosDe 173 pacientes evaluados, 171 casos fueron resecados, con una mortalidad del 1,2% y una morbilidad cardiorrespiratoria del 11,7%. La tasa de fallos del primer nivel del algoritmo fue del 4,6%, y del segundo nivel (prueba de esfuerzo) del 26%. La ausencia de prueba de esfuerzo se debió a problemas estructurales hospitalarios y a la incapacidad del paciente para realizarla. De los pacientes que se sometieron a esta prueba, 31 alcanzaron un VO2max de 20ml/kg-min o más y fueron intervenidos sin cálculo de los valores de FEV1ppo y DCLOppo; 35 precisaron de dicho cálculo para decidir su operabilidad, y en 2 casos no se recomendó la intervención por inoperabilidad funcional del paciente.
ConclusionesEn el 18,5% de los casos se han encontrado fallos en la aplicación del algoritmo, fundamentalmente por ausencia de la prueba de esfuerzo. La tasa de adecuación al algoritmo debe ser mejorada antes de poder realizar otros estudios de validación.
In 2009, the European Respiratory Society (ERS) and the European Society of Thoracic Surgery (ESTS) published clinical practice guidelines (CPG)1 that were the result of collaboration among specialists. These provided recommendations for a correct and detailed pretreatment assessment of patients with bronchogenic carcinoma. In particular, evidence was reviewed about the risks of lung resection, and the results were summarized in a preoperative evaluation algorithm in which each decision-making point is supported by a robust degree of evidence.
The objective of this study is to present an initial validation phase of the proposed pre-op evaluation process by quantifying the degree of compliance with the recommendations of the CPG in the actual clinical of a tertiary hospital.
MethodsA prospective, observational study developed between September 2009 and December 2010. Data were recorded for the 173 consecutive patients remitted for lung resection during the inclusion period. The cases basically came from six hospitals that regularly send cases to our hospital for surgery. Thus, before initiating the study, we had previously agreed upon the functional evaluation criteria with said centers in order to adapt them to European recommendations.
Throughout the study period, patients who were considered candidates for the preoperative evaluation had a Karnosfky index higher than 50%, did not present other systemic pathologies with a poorer prognosis than the tumor itself and imaging studies did not show the tumor to be unresectable.
According to the recommendations of the decision-making algorithm,1 three main levels of decision are established: general preoperative evaluation, physical exertion testing and calculation of the predicted postoperative values for several key variables in the preoperative evaluation. For each decision-making node, two or three exiting flow lines were established (depending on the level) to decide on either operability, the recommendation of a treatment as an alternative to surgery, or the need for other previous tests before making a definitive decision. The final node recommends either not to operate or to resect up to a certain lung extension, according to the calculation made.
Details of Each of the Algorithm Decision-making LevelsGeneral Preoperative StudyThe preoperative study that was agreed upon with each of the reference hospitals included hemogram, work-up with general chemistry and hepatic parameters, coagulation study, electrocardiogram, imaging tests (chest radiology and thoracic computed tomography [CT] with contrast) and, if necessary due to the oncological characteristics of the case, positron-emission tomography (PET-scan). If the patient presented known or suspected cardiologic pathology, a complete cardiologic evaluation was done. As for the functional respiratory evaluation, the patients should provide an evaluation of functional volumes (baseline spirometry and after bronchodilation in absolute values and age, sex and height percentiles) and a lung diffusion study (DLCO) with data for the diffusion of carbon monoxide adjusted for the hemoglobin value of the patient. In the spirometry evaluation, the key value is the FEV1% value, and in the diffusion study, the DLCO% adjusted for hemoglobin. Values greater than 80% enable the patient to undergo surgery without the need for any other tests. If either of the two values is lower, the patient requires an oxygen consumption test (preferably a high-tech test) before a decision is made.
Oxygen Uptake Testing (VO2max)With the data obtained from the functional respiratory evaluation, we can evaluate, following the proposed evaluation algorithm,1 the need for a high-tech exercise test that can only be carried out in our hospital by one trained specialist. The oxygen uptake test is done with a MasterScreen CPX module by Jaeger-Vyasis-Healthcare. From this test, we are able to obtain the data for oxygen consumption in absolute values (ml/kg-min) and peak (%), which will be used in later calculations, if necessary, so that patients with absolute values equal to or higher than 20ml/kg-min or with peak values equal to or higher than 75% can undergo surgery without any other tests and tolerate any type of resection. The patients with absolute values less than 10ml/kg-min or instead at 35% are classified as inoperable due to their high risk and an alternative treatment is recommended. Lastly, the group of patients with intermediate values need other calculations before making a decision.
Calculation of Predicted Post-op FEV1%, DLCO% and Peak VO2(%) ValuesAccording to the algorithm,1 in some cases it is necessary to follow the next assessment step, which is the calculation of the predicted postoperative values for lung function, contemplating both volume (FEV1%) as well as diffusion (DLCO%) and the values obtained from the exertion test: VO2max (ml/kg-min) and peak VO2(%) value. The calculations were done on two levels: first, the predicted post-op values are calculated for FEV1% and DLCO%, according to the resection proposed and, if one of said values is below 30%, it is then necessary to calculate the value of peak VO2(%) and VO2max. If in the end the VO2max were below 10ml/kg-min or estimated peak VO2(%) were below 35%, once again an alternative treatment would be recommended for the patient.
The calculation of said postoperative values is done following the formula published by Nakahara et al.2 In said formula, each segment is responsible for 5.26% of the recorded volumes. In addition, the formula takes into consideration the segments that need to be resected for an oncologically valid extirpation of the carcinoma and the segments that on bronchoscopy are obstructed by the tumor and which therefore do not intervene in the respiratory exchange.
Acquired VariablesIn this paper, we registered the presence or absence of the studies required (FEV1%, DLCO% adjusted for hemoglobin, VO2max [ml/kg-min], peak VO2%) and those that were calculated (FEV1ppo, DLCO%ppo, peak VO2ppo) for each level of the algorithm, the results and, if another test had not been done, the reason. Also provided are the hospital mortality and cardiorespiratory morbidity of the series. Finally, the adjustment data are given for each of the decision-making levels and the final rate of error in the validation of the application of the algorithm.
ResultsOut of the 173 patients evaluated for lung resection who met the basic requirements, 171 underwent surgery. The cardiorespiratory mortality rate for the series was 11.7%. Mortality was 1.2% (two patients); the two patients, who were 55 and 75 years old, presented with epidermoid lung carcinomas and had the common history of having been treated for laryngeal carcinomas: one received radiotherapy and the other underwent surgery. In the first case, the tumor, which was located in the upper right lobe and completely obstructed the lobe, affected the main carina, and therefore right pneumonectomy was performed with a resection of the tracheal carina. Functionally, the patient had good function and did not require oxygen uptake testing. The patient died 48h later after developing a post-pneumonectomy edema. The second patient died as a consequence of respiratory failure and right heart failure, which were irreversible in the context of pulmonary fibrosis that had been evolving over a long period of time. No treatment had been necessary, and the functional data were as follows: FEV1% 102%; DLCO% 70 and VO2max 19.8ml/kg-min. The estimated post-op values were: FEV1%ppo 74% and DLCOppo 51.6%. The patient underwent lower lobectomy.
In the first node of the algorithm, there was a non-compliance rate of 4.6% due to incompliance (eight patients) (Fig. 1). In one case, spirometry was not done and in six CO diffusion was not tested, while in one case both parameters were missing. We know that the tests were not done in eight cases due to technical problems: 8 patients were unable to correctly carry out the explorations required, and in the remaining case the reasons for the patient not doing either of the tests is unknown. The FEV1% and DLCO% values adjusted for hemoglobin were sufficient for 73 patients to undergo surgery without any other additional examination.
The exertion test—the following test in the decision-making flowchart—was done in 68 of the 92 patients for whom it was indicated (26% failure to comply). The causes due to which this test was not done were: in 14 cases, due to organizational reasons of the hospitals; in six cases, the test was contraindicated due to cardiovascular reasons; in three cases, due to the inability to perform the test due to knee joint limitations, and in the last case, due to vasovagal symptoms that impeded carrying out the test. With the data obtained from this test, 31 patients were able to undergo surgery without the need to complete any other studies, one patient was determined to be inoperable because of an oxygen consumption of less than 10ml/kg-min and in 36 cases it was necessary to continue with other calculations before deciding on operability.
After carrying out the calculations of the third decision-making node, 35 patients were able to be resected. One patient, with peak consumption below 35%, was considered to be functionally inoperable and an alternative treatment was recommended. In this node, there was no failure to acquire the calculation of the variables due to the characteristics of the node.
In summary, this means that in 81.5% of the cases (141/173) all the recommendations proposed in the guidelines were followed, while the algorithm was not complied with in 4.6% (8/173) of the cases in the first node and in 26% (24/92) of the patients requiring oxygen consumption calculation.
DiscussionWorking with clinical practice guidelines (CPG) entails using the best scientific evidence available for the benefit of our patients. But, in spite of their significance, CPG have not been universally implemented and they have not provided the expected results of continuous improvement in health-care quality. Failure to implement CPG has been reported at many levels: extrinsic of the guideline itself (e.g. organizational) or intrinsic (ambiguity, inconsistency or because the guidelines are incomplete, etc.).4 Due to the importance given to using CPG in standard practice, tools have been designed, such as the GLIA (GuideLine Implementability Appraisal), in order to better understand and anticipate the possible obstacles in the implementation and the development of any new CPG.3 International surveys5 have shown that many of the authors of CPG did not have a program for continuous improvements of the CPG created, and they lack personnel specifically dedicated to analyzing and spreading the use of CPG. Some think that it should be the receiving units that should be in charge of making analyses and improvements. This is one of the justifications for creating this study: to find out whether, in our setting and with the general conditions that we have available, it is possible to carry out the recommended protocol of preoperative assessment with sufficient rigor. Therefore, it is not a prediction study but instead only a descriptive study limited to the patients sent for evaluation. It is quite probable that there is selection bias prior to the patients being remitted for assessment due to decisions made at other levels that are beyond our knowledge and our control.
We know that applying the highest level scientific evidence to the preoperative evaluation is very important because surgical treatment of lung cancer offers more possibilities for a cure in early stages, but at the same it conditions a more important and more abrupt change in the quality of life of the patient. It is especially relevant to be able to rely on a tool that can distinguish between patients who can present with very important complications, even mortality, from those who, despite their comorbidity, may tolerate the procedure.1 According to a recent publication,6 the gross mortality of lung resection recorded in the European database of the ESTS, which includes data of more than 4000 patients, is 3%. In our series, the overall mortality rate is 1.2%. It is a mortality rate that is less than that of the European series, which shows a 2.9% gross mortality for surgical cases in Spain7 and suggests that it is a safe algorithm whose application can maintain mortality at a very low rate.
Out of the failures to comply that were detected in the application of the algorithm, possibly the most striking is the absence of lung function tests, which was seen in eight patients (4.6% of the series). Respiratory function testing should meet well-defined norms in order to guarantee a certain quality.8 Nevertheless, according to a recent Spanish article9 in which spirometry was done in a representative Spanish population between the ages of 65 and 85, some 10% of these studies may not be technically acceptable. This is a very important problem, as our estimations for surgical risk are based on spirometric volume measurements, specifically FEV1%, even with all the limitations of this parameter,1 and DLCO. It is possible that, in cases where it is technically impossible to perform valid lung function tests, patients should carry out exertion tests as an alternative and objective assessment of his/her risk.
The most important problem detected occurs at the level of the second decision-making node, where only 68 out of 92 patients (84%) performed the high-tech exercise test. It is considered the safest test for quantifying individual risk for postoperative complications.1 This technique, however, is not available in all the centers where lung surgery is done. When we reviewed the reasons for not carrying out the test, it should be noted that hospital organizational issues were responsible in 14 of the 24 cases that did not comply. Specifically, the organizational reasons included the fact that only one person was trained to administer and interpret the test, or technical problems/machine breakdowns made it impossible to do the test within a reasonable amount of time, so the test was not done so as not to prolong the wait indefinitely. It is possible that the solution to this problem is in the CPG itself,1 which considers the standardized test of climbing stairs to be limited by symptoms as an alternative to the high-tech lab test. The discriminative capability of this test may help reduce the number of patients that need laboratory tests. However, this test has been criticized due to its lack of standardization and the difficulty to perform it in a place that is safe for the patient.
Another interesting datum is that the impossibility of the patient to do the high-tech oxygen uptake test is also an important factor, responsible for 41.6% of the non-compliance in our series. Regarding this factor, cardiovascular contraindications (presented by six patients) and joint limitations (three patients) are especially relevant in a population that is getting older and older and, thus, has more comorbidities. It is very difficult to resolve this limitation. It is possible that new strategies need to be developed in order to be able to measure the exercise capacity of the patient without jeopardizing his/her safety by doing tests that cause great stress, such as measuring the distance walked and the quality of exercise that the patient does on a daily basis.10
In conclusion, by quantifying the degree of compliance with the recommendations included in the CPG for the preoperative assessment of surgical risk, we have detected a non-compliance rate of 18.5% in its application. 75% of this lack of compliance is seen in the second decision-making node because exertion tests are not performed, most of which (58.3% of cases) are due to hospital organizational problems.
Please cite this article as: Novoa NM, et al. Primera fase de validación del algoritmo europeo de evaluación funcional previa a la resección pulmonar: cuantificación del cumplimiento de las recomendaciones en la práctica clínica real. Arch Bronconeumol. 2012;48:229–33.