COVID-19, the infection caused by the SARS-CoV-2 virus, typically present with fever, cough, dyspnea, and myalgia, and the infection may cause severe pneumonia. Most of the patients with COVID-19 have mild disease symptoms. However, few patients can develop acute respiratory distress syndrome (ARDS) and other complications, including thrombotic phenomena.
The disease presents challenging clinical, pathophysiological, laboratory, and histopathological aspects that have been the subject of research in practically all countries in the world. This complexity of aspects also applies to imaging findings.
High-resolution chest CT is the most effective radiological examination for the evaluation of lung involvement by COVID-19. The predominant CT findings of COVID-19 pneumonia are multifocal, bilateral, peripheral, and basal-predominant ground-glass opacities, often with round and/or oval morphology and/or consolidation. The crazy-paving pattern may also be observed, particularly when the disease progresses. These CT findings are not specific to COVID-19; similar results can be obtained for other infectious and non-infectious diseases. Nonetheless, normal chest CT findings do not exclude this diagnosis.1–3
Another tomographycal finding recently related to COVID-19 pneumonia is the reversed halo sign (RHS). This sign is defined as a focal rounded area of ground-glass opacity surrounded by a complete or near-complete ring of consolidation observed on chest computed tomography,4 has been reported in association with a wide variety of clinical entities, including infectious and noninfectious diseases.5,6 The presence of the RHS in patients with COVID-19 has been reported,1,7–10 with a highly variable incidence among published studies. Bai et al.7 reported that the RHS was present in 5% of 219 patients, whereas the incidence was much lower in other casuistic studies; Bernheim et al.1 observed the RHS in only 1 of 121 patients, and Ai et al.3 did not report the presence of the sign in any of their 1014 patients. Although some authors have reported the appearance of the RHS in later stages of the disease, during the evolution of the pulmonary infectious process,1,2 other authors have described its presence in the first days after symptom onset.8,9
Recently a 48-year-old man presented to our hospital with a 5-day history of fever, cough and myalgia. He reported having systemic arterial hypertension and type 2 diabetes mellitus.
On admission, the patient was in good general condition; he was tachypneic, his body temperature was 38.2°C, and cardiac and pulmonary auscultation was normal. Laboratory tests showed a normal blood cell count, erythrocyte sedimentation rate of 96mm/h (normal=0–10mm/h), C-reactive protein level of 19mg/L (normal=0.3–10mg/L), and unremarkable lactate dehydrogenase, creatine phosphokinase, and liver function findings. Blood gas analysis yielded normal findings (O2 saturation=96%).
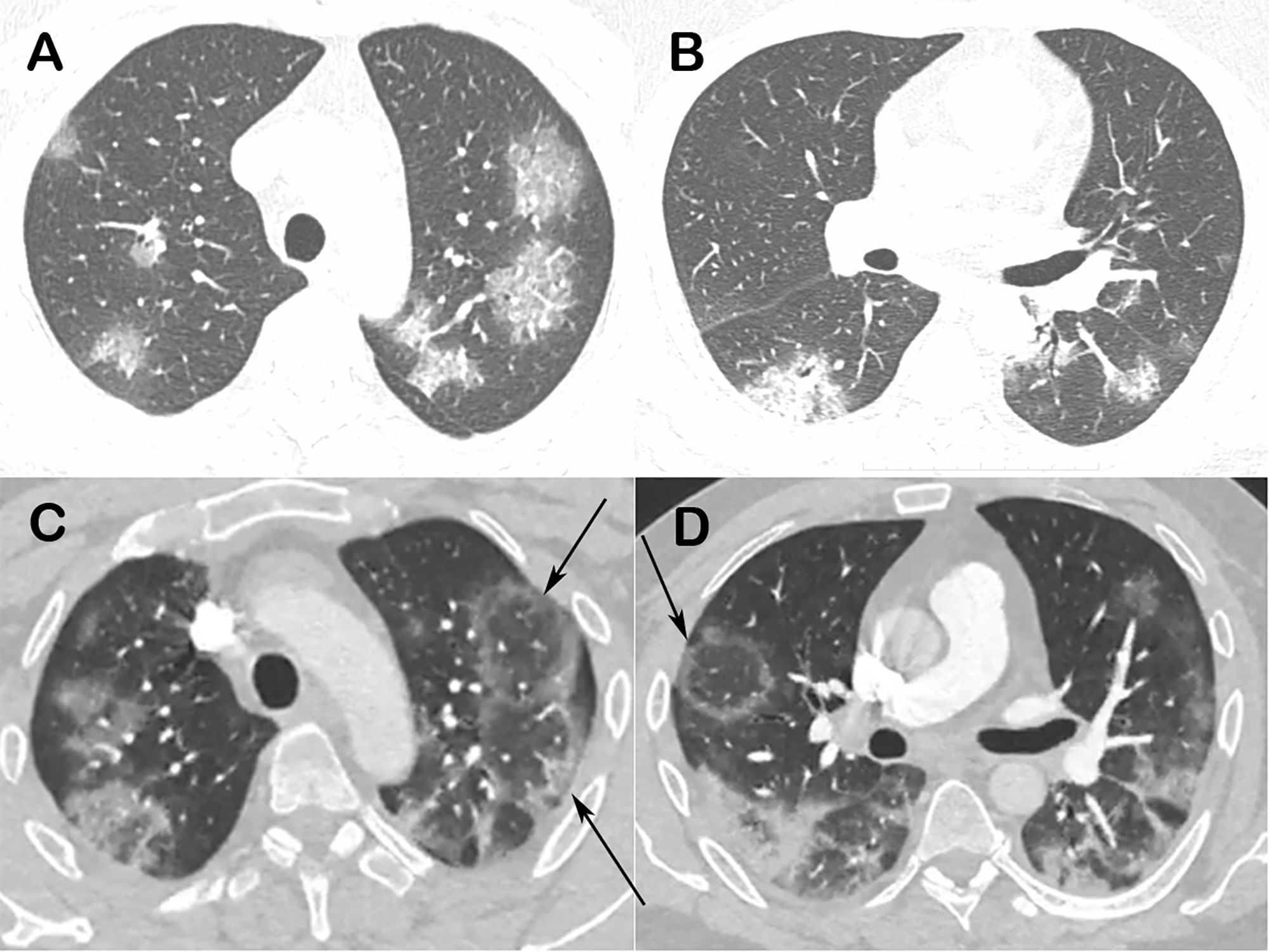
Real-time reverse-transcription polymerase chain reaction of a nasopharyngeal sample tested positive for the SARS-CoV-2, confirming the diagnosis of COVID-19. A chest computed tomography obtained 2 days after symptom onset showed bilateral ground-glass opacities (Fig. 1A and B). A new CT performed 3 days later demonstrated multiple RHS (Fig. 1C and D).
Chest computed tomography images of a 48-year-old man with confirmed COVID-19 pneumonia. Images obtained at the levels of the upper (A) and lower (B) lobes 2 days after symptom onset show bilateral round and oval ground-glass opacities. Enhanced images (C and D) obtained at the same levels as A and B 3 days later show multiple reversed halo signs (arrows) in both lungs.
Hydroxychloroquine and symptomatic medication were administered. The patient recovered uneventfully, with the disappearance of symptoms and normalization of laboratory tests. He was discharged after 14 days in an asymptomatic state.
To understand RHS formation, an understanding of the pathogenesis of lung injury is very important. Although few reports on the histopathological characteristics of COVID-19 have emerged to date, early stages of organization (fibroblast proliferation) have been observed to follow initial diffuse alveolar damage.11,12 Potential courses of this typical response to lung injury are known; if the stimulus for injury is removed and the basement membranes are intact, then the intraluminal fibroblastic tissue is remodeled into the interstitium or removed by the fibrinolytic system, and the normal architecture is re-established. If the stimulus for injury persists and the integrity of the basement membranes has been lost, then the alveoli collapse, their basement membranes fuse, fibroblast activation persists, and the self-reinforcing formation of organizing fibroblastic tissue progresses to fibrosis.13 In COVID-19 cases, the predomination of fibroblastic tissue organization and development of fibrosis have been observed after the first week of the symptom onset. This process can be characterized as organizing pneumonia, which appears histologically as organizing fibroblastic plugs of spindle-shaped cells in a pale-staining matrix.13 Also, presence of alveolar exudative inflammation, interstitial inflammation, fibrin exudation and alveolar hemorrhage has been described, and can compose the appearance of ground glass opacities seen in the RHS.14,15 Consistently, histopathological examination of a transthoracic-needle lung biopsy sample from a patient who died 3 weeks after COVID-19 diagnosis showed diffuse alveolar damage in the organizing phase, with intra-alveolar fibrinous exudates, interstitial fibrosis, intra-alveolar fibrous plugs and organizing fibrin at most foci.12
This finding suggests that the disease course of COVID-19 might be similar to those of other viral infections, with early progression to organizing pneumonia and presentation of the RHS.
Conflicts of interestsThe authors declare that they have no conflicts of interest to express.