The aim of present study is to compare the effectiveness, side-effect potential of different doses of sericin pleurodesis.
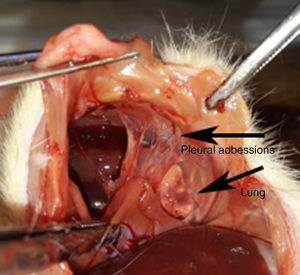
MethodsAdult, male, 12-week-old, Wistar-albino rats (n=52), were randomly-divided into four-groups, referred to A, B, C and D. Sericin was administrated at different doses through left thoracotomy, with 15mg sericin to Group-A, 30mg to Group-B and 45mg to Group-C. Group-D was assigned as control group. The rats were sacrificed 12 days later. Left-hemithorax, heart, liver and kidney were examined pathologically.
ResultsNo foreign body reaction in the parenchyma was observed in any of the rats, while emphysema was least common in Group-B (P<.05). Multi-layer mesothelium of both pleura was most common in Group-B, while fibrosis and fibrin organization within the visceral-pleura was more successful in all of sericin treated groups than in control group (P<.05), with neither Group-A, Group-B nor Group-C being superior to each other. In the examination of collagen fibers using Masson's trichrome, “dense collagen fibers” were found in all three sericin treated groups, and differences between Groups-A, -B, -C and the control group were significant (P<.05). The probability of observing pyknotic nucleus and balloon degeneration in liver increased with increasing sericin doses (P<.05). Glomerular degeneration in kidney and the findings of pericarditis were most common in Group-C (P<.05).
ConclusionThe target should be to maximize efficacy while minimizing the likelihood of side-effects. The intrapleural administration of sericin 30mg performs better due to multi-layer mesothelial reaction being higher and emphysema being lower in Group-B, to the fewer side-effects affecting the kidney and heart, and liver toxicity not being higher.
El objetivo de este estudio es comparar la efectividad y los posibles efectos secundarios de diferentes dosis del agente pleurodésico sericina.
MétodosSe utilizaron ratas macho albinas Wistar de 12 meses de edad (n=52) que se dividieron aleatoriamente en 4 grupos, referidos como A, B, C y D. Se administró sericina a diferentes dosis a través de toracotomía izquierda: 15mg al grupo A, 30mg al grupo B y 45mg al grupo C. El grupo D se utilizó como grupo control. Las ratas se sacrificaron 12 días más tarde. Se realizó examen patológico del hemitórax izquierdo, el hígado y el riñón.
ResultadosNo se observaron reacciones a cuerpo extraño en el parénquima de ninguna de las ratas. El enfisema fue menos común en el grupo B (p<0,05). El mesotelio multicapa en ambas pleuras fue más frecuente en el grupo B, mientras que la fibrosis y la organización de la fibrina en la pleura visceral tuvieron una mayor tasa de éxito en todos los grupos tratados con sericina que en el control (p<0,05), sin ser mayor en ninguno de los grupos. Cuando se examinaron las fibras de colágeno mediante el tricrómico de Masson, se encontraron «fibras densas de colágeno» en los 3 grupos tratados con sericina, existiendo diferencias significativas entre los grupos A, B y C (p<0,05). La probabilidad de observar núcleos picnóticos y degeneración «en globo» en el hígado se incrementó con el aumento de las dosis de sericina (p<0,05). La degeneración glomerular en el riñón, y los hallazgos de pericarditis fueron más frecuentes en el grupo C (p<0,05).
ConclusiónEl objetivo debería ser maximizar la eficacia a la vez que se minimiza la probabilidad de efectos secundarios. La administración intrapleural de 30mg de sericina resulta más eficaz debido a una mayor reacción mesotelial multicapa y a menor incidencia de enfisema (como se observa en el grupo B), así como a un menor número de efectos adversos que afectan al riñón y al corazón sin incremento concomitante de la toxicidad hepática.
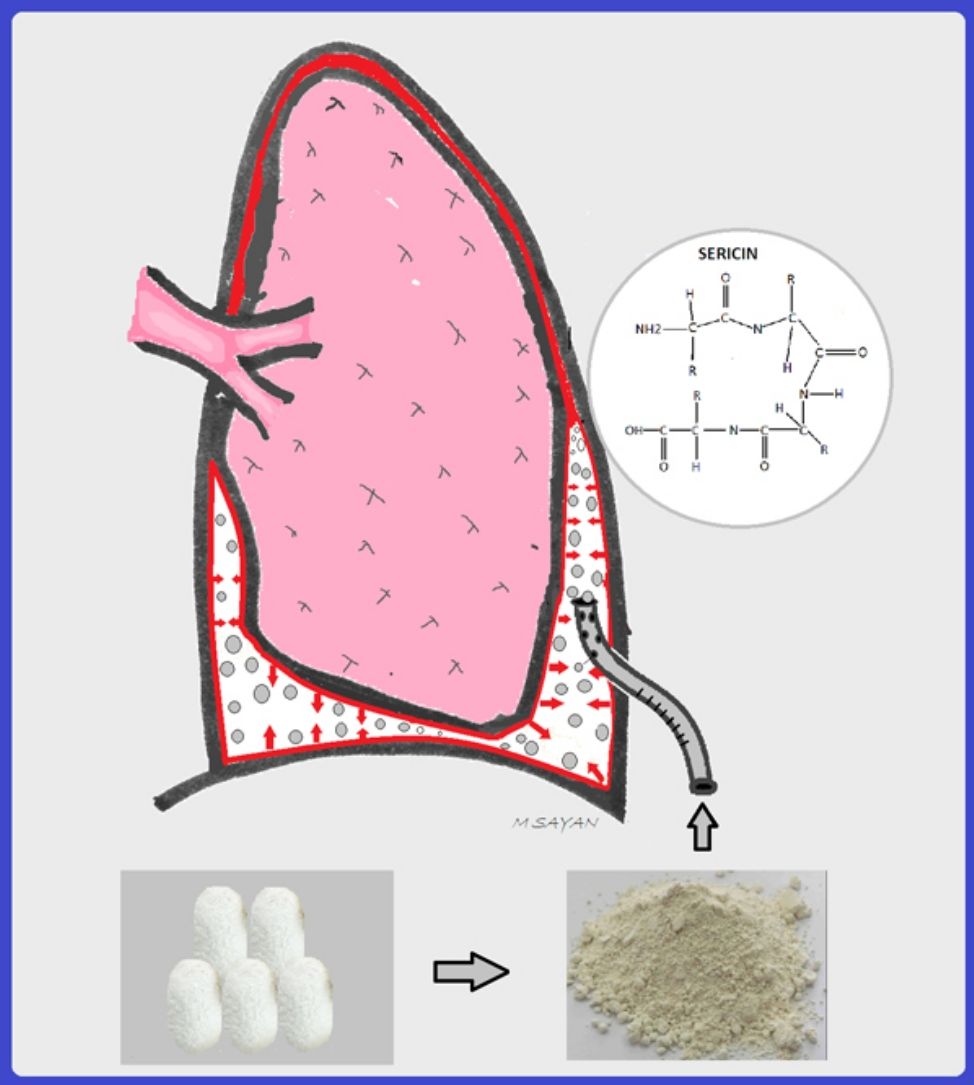
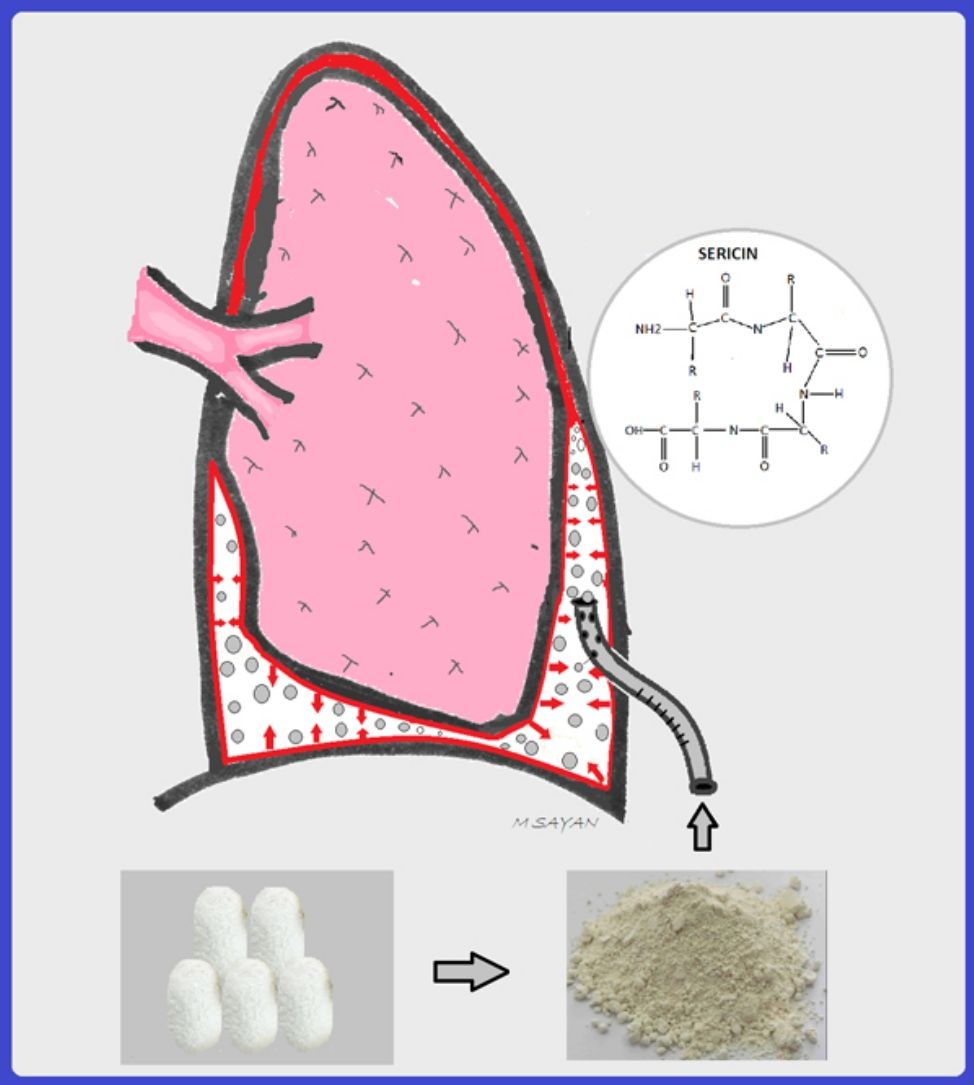
Sericin is a gum-like and natural protein which holds fibroin polymers together for reconstruction of the cocoon shell of the silkworm Bombyx mori.1 The removal of sericin from cocoon is accomplished using a specialized process called “degumming”.2 Sericin has many applications in the field of science, such as an antiwrinkle, antiaging, antioxidant, and antimicrobial agent thanks to its strong polar side groups, as well as an additive on cell culture media to enhance cell movement and proliferation.3–8 Sericin, also has a cholesterol-lowering effect in high-cholesterol fed rats and anticancer effects via inducing apoptosis of human lung and colon cancer cells.9–11 Finally, sericin has a healing effect on skin wounds and enhances the proliferation of fibroblasts, which play a key role in the healing process.12–14
Pleurodesis is the symphysis between the visceral and parietal pleura which prevents the accumulation of either air or liquid in the pleural space. Yazicioglu et al. demonstrated the usefulness of sericin as a pleurodesis agent.15 In another study, sericin pleurodesis was compared with talcum powder, doxycycline, and silver nitrate pleurodesis and the authors showed that sericin pleurodesis resulted in the highest levels of dense collagen fibers in the pleura with superior pulmonary safety profile and a lower potential for inflammation.16 In addition, adverse effects concerning the kidneys and heart were significantly lower in the sericin treated group than the other pleurodesis groups.16
However, to date there is no comparative study investigating different doses of sericin for pleurodesis. Previous studies used 30mg sericin for pleurodesis, and the effects of other doses have not been well-established, yet. In the present study, we aimed to investigate whether lower doses of sericin were also effective and whether higher doses were harmful for the lung parenchyma and other organs. We believe that the investigation of different sericin doses is an important step in the process of making it commercially available.
Materials and methodsAn animal study was designed to compare the effectiveness and safety of different doses of sericin pleurodesis. The rat model was selected due to the presence of a valid laboratory license, technical feasibility, and similar physiological characteristics of rats with humans. The sericin powder which is commercially available was purchased from Xi’an Lyphar Biotech Co., Ltd., Xi’an, China. In the studies of Yazicioglu et al., 30mg sericin application resulted in successful pleurodesis in 220–395g rats. In the present study, we compared different sericin doses, 15mg, 30mg, and 45mg.
AnimalsThe animal study was approved by the Ethics Committee of Kobay AS (Protocol Number-239/2017). A total of 52 adult, male, 12-week-old Wistar albino rats weighing between 234 and 317g were used. The rats were randomly divided into four groups in equal numbers, including 13 in each group: 15mg (Group-A), 30mg (Group-B), and 45mg (Group-C), and sham thoracotomy group (Group-D). All of the animals received humane care in accordance with Turkish Government Animal Protection and Management Law.
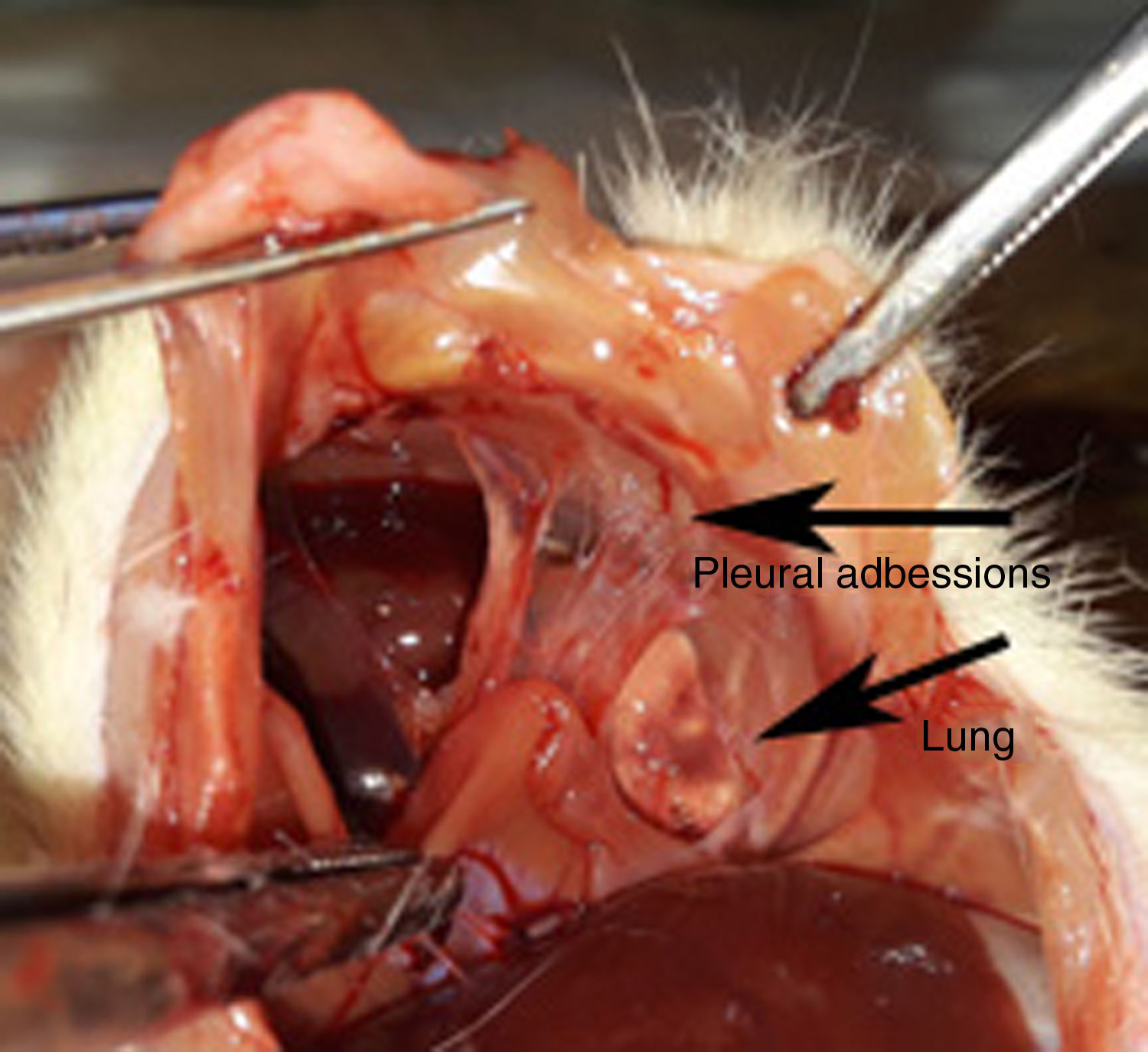
TechniqueThe sericin powder was divided into 15mg, 30mg, 45mg packs, and added into Eppendorf tubes. The operation and post-operative conditions of rats was performed following instructions previously described by Yazicioglu et al.15 Sericin was administrated to the left hemithorax of rats in suspension form. All the rats were weighed before surgery and before scarification, and the respective body weights were recorded.
The rats were sacrificed at postoperative day 12; cardiac puncture was the preferred method. The left hemithorax was removed en-bloc, the lungs were fully expanded and the trachea was ligated. The entire hemithorax with the heart and additionally the liver and kidney were removed and submerged in a 10% formaldehyde solution, and samples were submitted to the pathology laboratory.
Pathological examinationFor microscopic evaluation, representative tissue sections of the visceral and parietal pleura, lung parenchyma, thoracic wall, liver, kidney, and heart were prepared. These samples were processed through a graded mixture of alcohol and xylene, and embedded in paraffin blocks and 6-μm tissue sections were obtained and stained with hematoxylin eosin (HE) and Masson's trichrome. The pathologist (investigator F.D.) was kept blind to the study groups and sections were evaluated using light microscopy (Olympus BX53). Particular attention was given to the parameters of the lung parenchyma, thoracic wall, parietal and visceral pleura, liver, kidney, and the heart. Collagen deposition was evaluated using Masson's trichrome stain.
In the pathological evaluation of the tissues a semi-quantitative method was preferred. The parameters of foreign body reaction, presence of biologic glue, emphysema, organizing fibrin on pleura, and potential side-effects were classified as “none” or “yes”. The pathological slides were graded for inflammation/cellularity and scored using the following system developed by Hurewitz et al., and classified as “none”, “mild”, “moderate”, and “severe”.17 The degree of fibrosis was scored using the following system developed by Vargas et al., and classified as “none”, “mild”, “moderate”, and “severe”.18 The evaluation of Masson's trichrome staining was classified as “none”, “sparse”, and “dense”. Collagen fibers were classified as “sparse” if the fibers are thin, sparse and in small number, and as “dense” if the fibers are thick and widespread.
Statistical analysesThe pathologic data were expressed using statistical analyses, which were conducted using the SPSS statistical software package (version 17.0, SPSS, Chicago, IL, United States). The one-way ANOVA test was used to analyze the potential differences between study groups. In cases where a difference was detected between the groups, the Levene test was used to check the differences between the variances and to identify which group was the source of difference. The variances were not equal when P values were <.05 based on the Levene tests, and the Tamhane's and Dunnett's t-test were used in such cases. Variances were considered equal when P values were > .05 based on the Levene test, and Scheffe test was used in such circumstances. For most of the parameters included in the statistical analyses, the Levene test result was P<.05. Thus, the variances were found to be unequal, and the Tamhane's and Dunnett's t-test were used. Based on Scheffe, Tamhane's and Dunnett's t-tests, P values of < .05 were considered statistically significant.19
ResultsOnly one animal in Group-C died within the first 24h following surgery. In this case, the cause of death was considered to be a complication of the anesthesia and autopsy samples were not obtained. The remaining 51 rats completed the study and were sacrificed on Day 12.
The body weight of the rats was measured before surgery and scarification, and the data were compared. While all rats in Group-B gained weight, six rats (46.2%) in Group-A and one rat (8.3%) in Group-C lost weight during the postoperative period. The mean weight gain among the rats in the Groups-A, -B, -C, and -D was 8.1g (range: 4–18g), 34.9g (range: 13–60g), 30.8g (range: 15–56g), and 18.3g (range: 7–44g), respectively. In terms of the mean weight, the procedure was better tolerated by the rats in Group-B and Group-C, and the highest weight gain was recorded in these groups. The Scheffe's test indicated that the mean weight loss in the Group-A was significantly higher compared to the other groups (Group-A vs. Group-B (P=.01); Group-A vs. Group-C (P=.01); Group-A vs. Group-D (P=.04)).
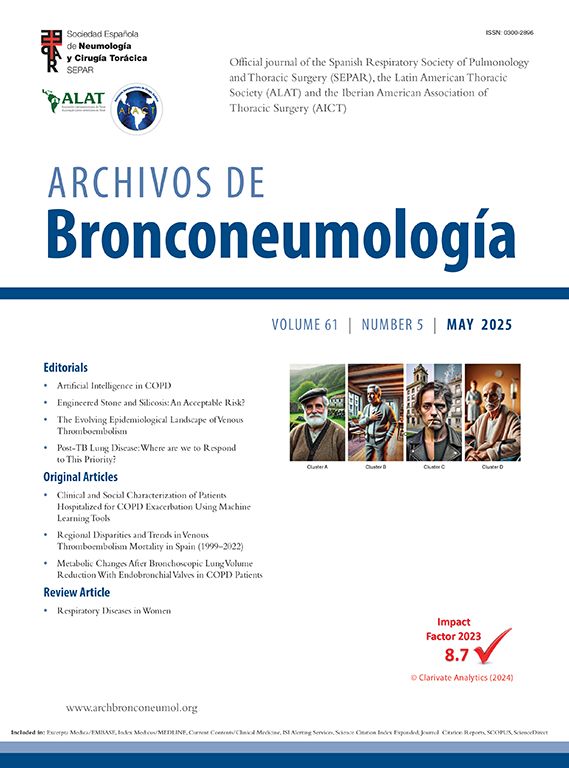
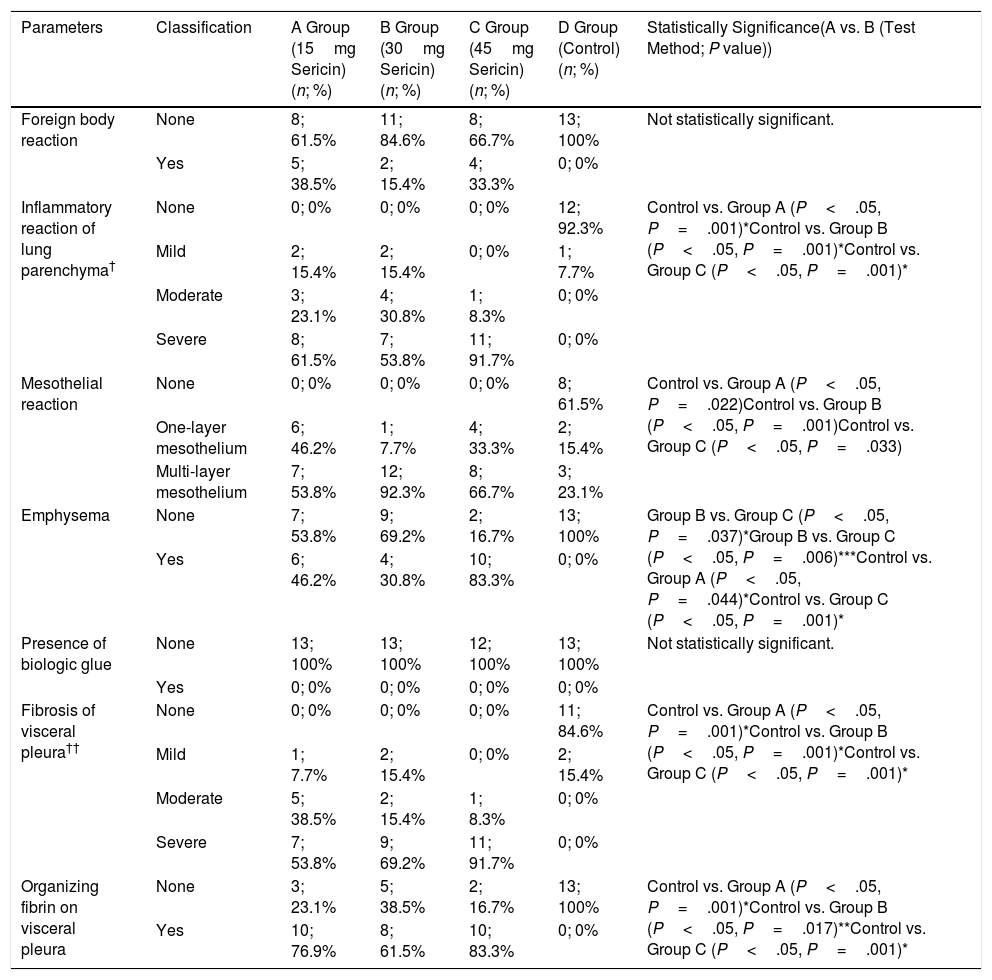
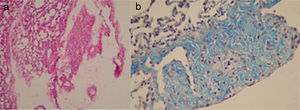
The evaluation of lung parenchyma and visceral pleuraThe rates of foreign body reaction and inflammatory reaction were similar in all groups. The likelihood of emphysema increased in parallel with the sericin dose and Group-C had the highest rate (P<.05) (Fig. 1a). A significant mesothelial reaction was observed in all of the groups (P<.05). Multi-layer mesothelium was most frequently seen in Group-B (Fig. 1b). Fibrosis and fibrin organization in the visceral pleura was achieved in all of the sericin groups to a significantly greater extent than that in Group-D (P<.05 for each comparison) (Fig. 2a). The results are detailed in Table 1.
The evaluation of lung parenchyma and visceral pleura.
| Parameters | Classification | A Group (15mg Sericin)(n; %) | B Group (30mg Sericin)(n; %) | C Group (45mg Sericin) (n; %) | D Group (Control)(n; %) | Statistically Significance(A vs. B (Test Method; P value)) |
|---|---|---|---|---|---|---|
| Foreign body reaction | None | 8; 61.5% | 11; 84.6% | 8; 66.7% | 13; 100% | Not statistically significant. |
| Yes | 5; 38.5% | 2; 15.4% | 4; 33.3% | 0; 0% | ||
| Inflammatory reaction of lung parenchyma† | None | 0; 0% | 0; 0% | 0; 0% | 12; 92.3% | Control vs. Group A (P<.05, P=.001)*Control vs. Group B (P<.05, P=.001)*Control vs. Group C (P<.05, P=.001)* |
| Mild | 2; 15.4% | 2; 15.4% | 0; 0% | 1; 7.7% | ||
| Moderate | 3; 23.1% | 4; 30.8% | 1; 8.3% | 0; 0% | ||
| Severe | 8; 61.5% | 7; 53.8% | 11; 91.7% | 0; 0% | ||
| Mesothelial reaction | None | 0; 0% | 0; 0% | 0; 0% | 8; 61.5% | Control vs. Group A (P<.05, P=.022)Control vs. Group B (P<.05, P=.001)Control vs. Group C (P<.05, P=.033) |
| One-layer mesothelium | 6; 46.2% | 1; 7.7% | 4; 33.3% | 2; 15.4% | ||
| Multi-layer mesothelium | 7; 53.8% | 12; 92.3% | 8; 66.7% | 3; 23.1% | ||
| Emphysema | None | 7; 53.8% | 9; 69.2% | 2; 16.7% | 13; 100% | Group B vs. Group C (P<.05, P=.037)*Group B vs. Group C (P<.05, P=.006)***Control vs. Group A (P<.05, P=.044)*Control vs. Group C (P<.05, P=.001)* |
| Yes | 6; 46.2% | 4; 30.8% | 10; 83.3% | 0; 0% | ||
| Presence of biologic glue | None | 13; 100% | 13; 100% | 12; 100% | 13; 100% | Not statistically significant. |
| Yes | 0; 0% | 0; 0% | 0; 0% | 0; 0% | ||
| Fibrosis of visceral pleura†† | None | 0; 0% | 0; 0% | 0; 0% | 11; 84.6% | Control vs. Group A (P<.05, P=.001)*Control vs. Group B (P<.05, P=.001)*Control vs. Group C (P<.05, P=.001)* |
| Mild | 1; 7.7% | 2; 15.4% | 0; 0% | 2; 15.4% | ||
| Moderate | 5; 38.5% | 2; 15.4% | 1; 8.3% | 0; 0% | ||
| Severe | 7; 53.8% | 9; 69.2% | 11; 91.7% | 0; 0% | ||
| Organizing fibrin on visceral pleura | None | 3; 23.1% | 5; 38.5% | 2; 16.7% | 13; 100% | Control vs. Group A (P<.05, P=.001)*Control vs. Group B (P<.05, P=.017)**Control vs. Group C (P<.05, P=.001)* |
| Yes | 10; 76.9% | 8; 61.5% | 10; 83.3% | 0; 0% |
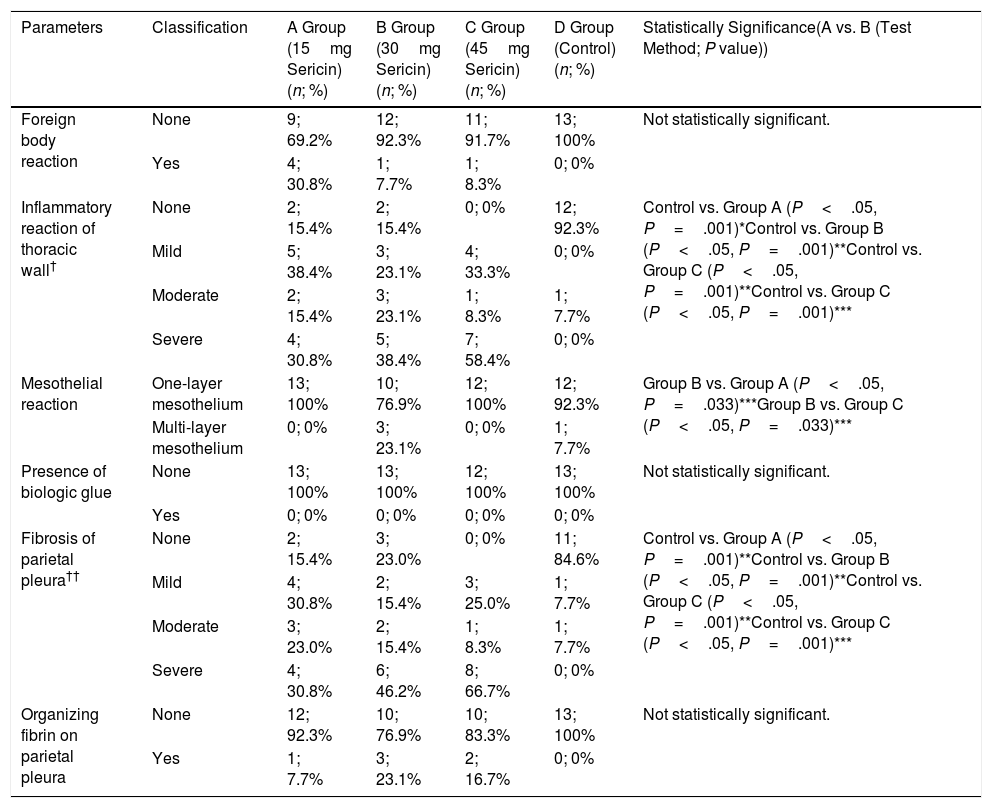
Foreign body reaction and inflammatory reaction were observed in a similar rate in all groups. Biological glue was not detected in any tissue of the rats. Multi-layer mesothelium was most frequently seen in Group-B (P<.05). Fibrosis and fibrin organization in the parietal pleura was achieved in all of the sericin groups to a significantly greater extent than that in Group-D (P<.05 for each comparison). The results are detailed in Table 2.
The evaluation of parietal pleura and thoracic wall.
| Parameters | Classification | A Group (15mg Sericin)(n; %) | B Group (30mg Sericin)(n; %) | C Group (45mg Sericin)(n; %) | D Group (Control)(n; %) | Statistically Significance(A vs. B (Test Method; P value)) |
|---|---|---|---|---|---|---|
| Foreign body reaction | None | 9; 69.2% | 12; 92.3% | 11; 91.7% | 13; 100% | Not statistically significant. |
| Yes | 4; 30.8% | 1; 7.7% | 1; 8.3% | 0; 0% | ||
| Inflammatory reaction of thoracic wall† | None | 2; 15.4% | 2; 15.4% | 0; 0% | 12; 92.3% | Control vs. Group A (P<.05, P=.001)*Control vs. Group B (P<.05, P=.001)**Control vs. Group C (P<.05, P=.001)**Control vs. Group C (P<.05, P=.001)*** |
| Mild | 5; 38.4% | 3; 23.1% | 4; 33.3% | 0; 0% | ||
| Moderate | 2; 15.4% | 3; 23.1% | 1; 8.3% | 1; 7.7% | ||
| Severe | 4; 30.8% | 5; 38.4% | 7; 58.4% | 0; 0% | ||
| Mesothelial reaction | One-layer mesothelium | 13; 100% | 10; 76.9% | 12; 100% | 12; 92.3% | Group B vs. Group A (P<.05, P=.033)***Group B vs. Group C (P<.05, P=.033)*** |
| Multi-layer mesothelium | 0; 0% | 3; 23.1% | 0; 0% | 1; 7.7% | ||
| Presence of biologic glue | None | 13; 100% | 13; 100% | 12; 100% | 13; 100% | Not statistically significant. |
| Yes | 0; 0% | 0; 0% | 0; 0% | 0; 0% | ||
| Fibrosis of parietal pleura†† | None | 2; 15.4% | 3; 23.0% | 0; 0% | 11; 84.6% | Control vs. Group A (P<.05, P=.001)**Control vs. Group B (P<.05, P=.001)**Control vs. Group C (P<.05, P=.001)**Control vs. Group C (P<.05, P=.001)*** |
| Mild | 4; 30.8% | 2; 15.4% | 3; 25.0% | 1; 7.7% | ||
| Moderate | 3; 23.0% | 2; 15.4% | 1; 8.3% | 1; 7.7% | ||
| Severe | 4; 30.8% | 6; 46.2% | 8; 66.7% | 0; 0% | ||
| Organizing fibrin on parietal pleura | None | 12; 92.3% | 10; 76.9% | 10; 83.3% | 13; 100% | Not statistically significant. |
| Yes | 1; 7.7% | 3; 23.1% | 2; 16.7% | 0; 0% |
The number of subjects in some groups was insufficient for statistical analysis; groups with moderate and severe inflammation were combined. Statistical analyses were performed based on the groups determined with no inflammation, mild inflammation, moderate+severe inflammation in the thoracic wall.
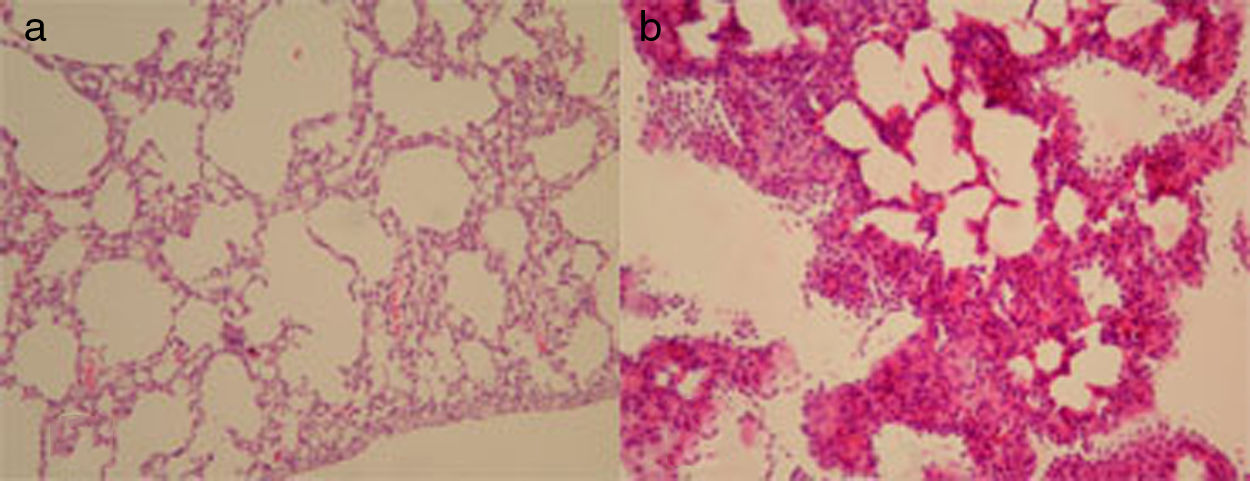
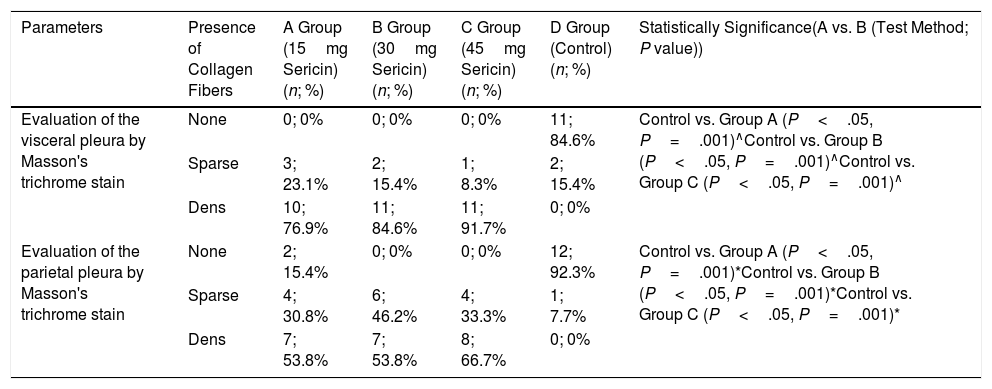
The Masson's trichrome staining was used to evaluate the collagen fibers in the pleurae. The collagen fibers in the parietal and visceral pleura were more dense in all of the sericin groups compared to Group-D (P<.05) (Fig. 2b). However, there was no statistically significant difference among the groups. The results are detailed in Table 3.
The evaluation of masson's trichrome staining of parietal and visceral pleura.
| Parameters | Presence of Collagen Fibers | A Group (15mg Sericin)(n; %) | B Group (30mg Sericin)(n; %) | C Group (45mg Sericin)(n; %) | D Group (Control)(n; %) | Statistically Significance(A vs. B (Test Method; P value)) |
|---|---|---|---|---|---|---|
| Evaluation of the visceral pleura by Masson's trichrome stain | None | 0; 0% | 0; 0% | 0; 0% | 11; 84.6% | Control vs. Group A (P<.05, P=.001)∧Control vs. Group B (P<.05, P=.001)∧Control vs. Group C (P<.05, P=.001)∧ |
| Sparse | 3; 23.1% | 2; 15.4% | 1; 8.3% | 2; 15.4% | ||
| Dens | 10; 76.9% | 11; 84.6% | 11; 91.7% | 0; 0% | ||
| Evaluation of the parietal pleura by Masson's trichrome stain | None | 2; 15.4% | 0; 0% | 0; 0% | 12; 92.3% | Control vs. Group A (P<.05, P=.001)*Control vs. Group B (P<.05, P=.001)*Control vs. Group C (P<.05, P=.001)* |
| Sparse | 4; 30.8% | 6; 46.2% | 4; 33.3% | 1; 7.7% | ||
| Dens | 7; 53.8% | 7; 53.8% | 8; 66.7% | 0; 0% |
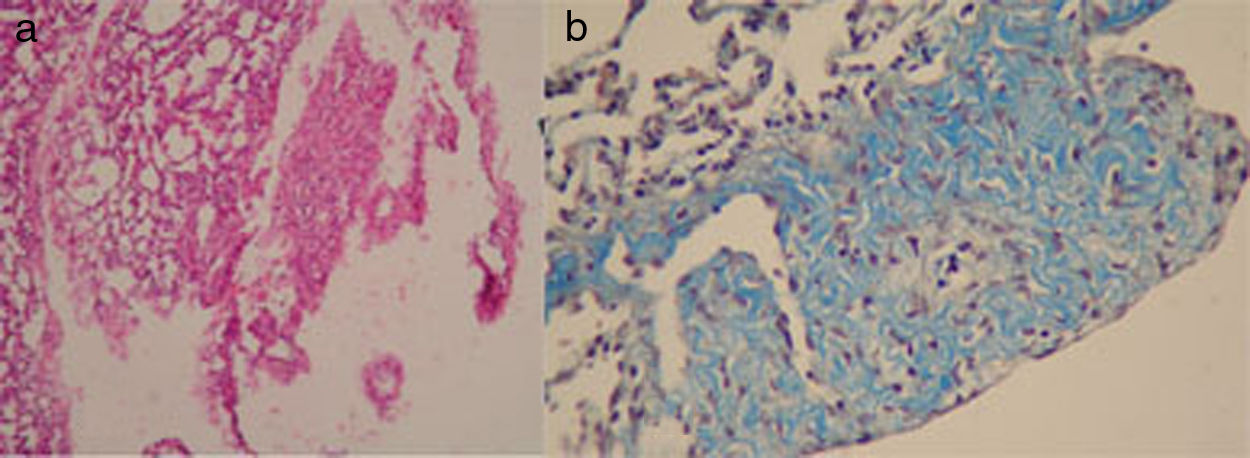
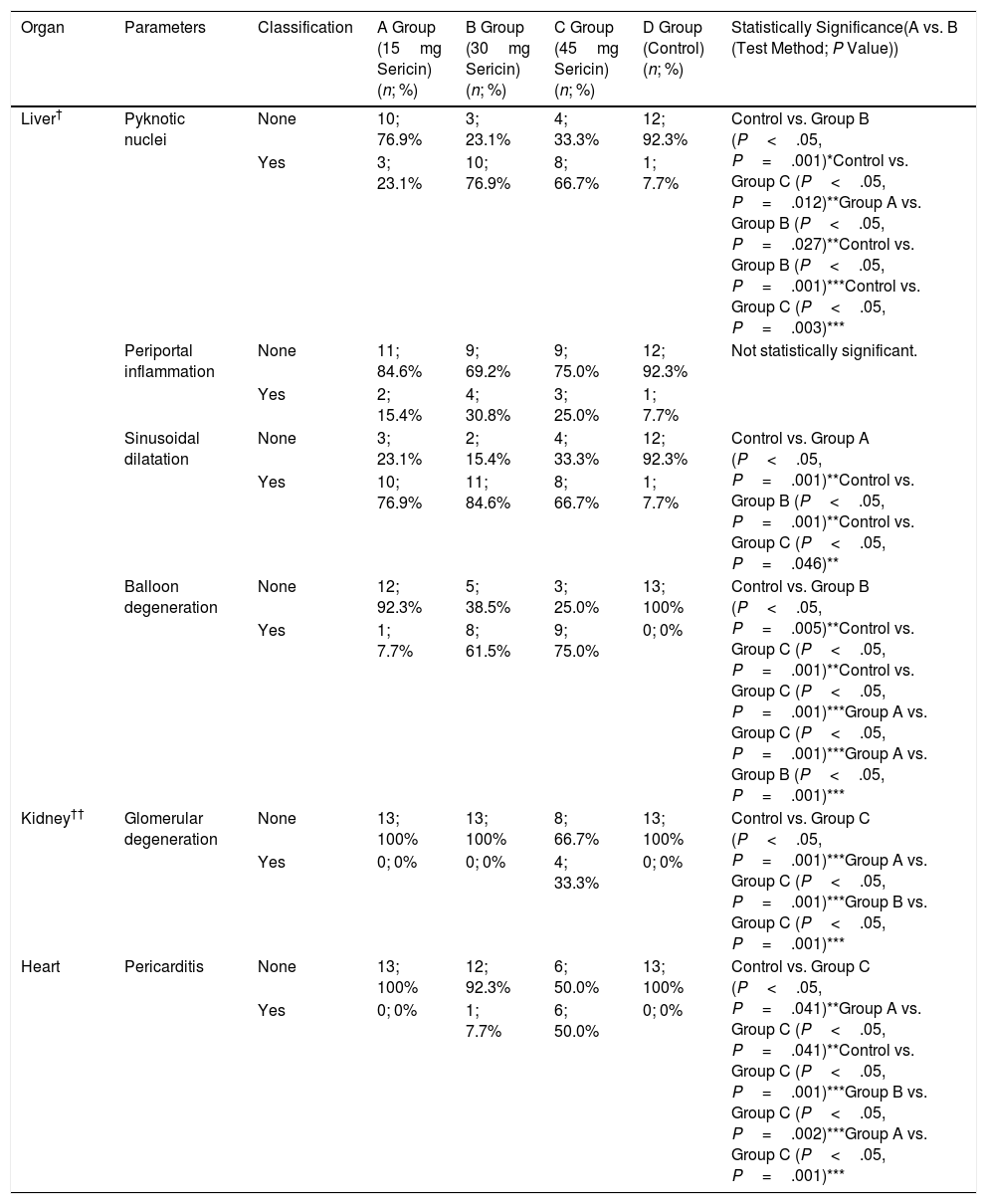
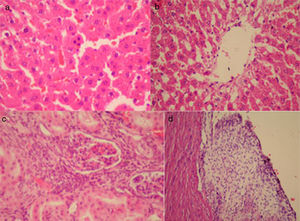
While sericin administration increased the likelihood of pyknotic nuclei and ballooning degeneration in the liver in a dose dependent manner, significant sinusoidal dilatation was observed in all of the sericin groups (P<.05) (Fig. 3a and b). In the kidney, glomerular degeneration was more common in Group-C compared to the other groups (P<.05) (Fig. 3c). Pericarditis was also more common in Group-C compared to the other groups (P<.05) (Fig. 3d). The results are detailed in Table 4.
The evaluation of liver, kidney, heart and pericardium after pleurodesis.
| Organ | Parameters | Classification | A Group (15mg Sericin)(n; %) | B Group (30mg Sericin)(n; %) | C Group (45mg Sericin)(n; %) | D Group (Control)(n; %) | Statistically Significance(A vs. B (Test Method; P Value)) |
|---|---|---|---|---|---|---|---|
| Liver† | Pyknotic nuclei | None | 10; 76.9% | 3; 23.1% | 4; 33.3% | 12; 92.3% | Control vs. Group B (P<.05, P=.001)*Control vs. Group C (P<.05, P=.012)**Group A vs. Group B (P<.05, P=.027)**Control vs. Group B (P<.05, P=.001)***Control vs. Group C (P<.05, P=.003)*** |
| Yes | 3; 23.1% | 10; 76.9% | 8; 66.7% | 1; 7.7% | |||
| Periportal inflammation | None | 11; 84.6% | 9; 69.2% | 9; 75.0% | 12; 92.3% | Not statistically significant. | |
| Yes | 2; 15.4% | 4; 30.8% | 3; 25.0% | 1; 7.7% | |||
| Sinusoidal dilatation | None | 3; 23.1% | 2; 15.4% | 4; 33.3% | 12; 92.3% | Control vs. Group A (P<.05, P=.001)**Control vs. Group B (P<.05, P=.001)**Control vs. Group C (P<.05, P=.046)** | |
| Yes | 10; 76.9% | 11; 84.6% | 8; 66.7% | 1; 7.7% | |||
| Balloon degeneration | None | 12; 92.3% | 5; 38.5% | 3; 25.0% | 13; 100% | Control vs. Group B (P<.05, P=.005)**Control vs. Group C (P<.05, P=.001)**Control vs. Group C (P<.05, P=.001)***Group A vs. Group C (P<.05, P=.001)***Group A vs. Group B (P<.05, P=.001)*** | |
| Yes | 1; 7.7% | 8; 61.5% | 9; 75.0% | 0; 0% | |||
| Kidney†† | Glomerular degeneration | None | 13; 100% | 13; 100% | 8; 66.7% | 13; 100% | Control vs. Group C (P<.05, P=.001)***Group A vs. Group C (P<.05, P=.001)***Group B vs. Group C (P<.05, P=.001)*** |
| Yes | 0; 0% | 0; 0% | 4; 33.3% | 0; 0% | |||
| Heart | Pericarditis | None | 13; 100% | 12; 92.3% | 6; 50.0% | 13; 100% | Control vs. Group C (P<.05, P=.041)**Group A vs. Group C (P<.05, P=.041)**Control vs. Group C (P<.05, P=.001)***Group B vs. Group C (P<.05, P=.002)***Group A vs. Group C (P<.05, P=.001)*** |
| Yes | 0; 0% | 1; 7.7% | 6; 50.0% | 0; 0% |
Sericin has many applications, such as an anti-wrinkle, anti-aging, antioxidant, and antimicrobial use. As an additive for cell culture media it has also a healing effect on skin wounds and enhances the proliferation of fibroblasts.3–14 On the other hand, sericin has in vitro natural glue properties. Liang et al. demonstrated that gelatin/sericin/carboxymethyl chitosan solution was effective as tissue glue with a low cost and excellent biocompatibility.20
Similarly, Yazicioglu et al. conducted an experimental study to investigate the effectiveness of intrapleural sericin administration on the fusion of both pleural sheets. In this study, the authors concluded that the intrapleural administration of sericin increased the fibroblastic activity and fibrosis in the visceral pleura without any significant adverse effects on the lung parenchyma.15 There were no evidence of foreign body reactions or evidence of biological glue on the specimens in the sericin pleurodesis group, and the rats in this group had lower inflammatory reactions compared to the control group.15 Sericin pleurodesis was compared with the other available pleurodesis agents such as talcum powder, doxycycline, and silver nitrate in another study.16 In this study, the authors reported that sericin was a cost-effective and well-tolerated agent by the rats and it successfully led to pleurodesis without any adverse effects on the lung parenchyma.16 As it is an intrinsic protein, foreign body reactions and emphysema were less common in the sericin group compared to the talcum powder and doxycycline groups (P<.05).16
Studies are ongoing worldwide to discover natural and cost-effective novel pleurodesis agents with higher effectiveness and improved safety profile.21 An ideal pleurodesis agent must be safe, widely available, inexpensive, and easily administrated. However, there is no agent on which a wide-held consensus has been obtained. Sericin is new protein with potential use in research and in thoracic surgery and pulmonology practice. However, to the best of our knowledge, there is no study available in the literature comparing different doses of sericin pleurodesis in terms of effectiveness and side effects.
Sericin has good tissue protective features and enhances wound repair.12–14 In the present study, there was no evidence of biological glue in any of the tissues tested among the sericin administrated groups. Therefore, even high doses of sericin do not seem to cause the presence of biological glue in tissues (Tables 1 and 2). Furthermore, foreign body reactions were similar in the study groups (Tables 1 and 2). These findings are in consistent with the study of Yazicioglu et al. which compared sericin with talcum powder, doxycycline, and silver nitrate.16
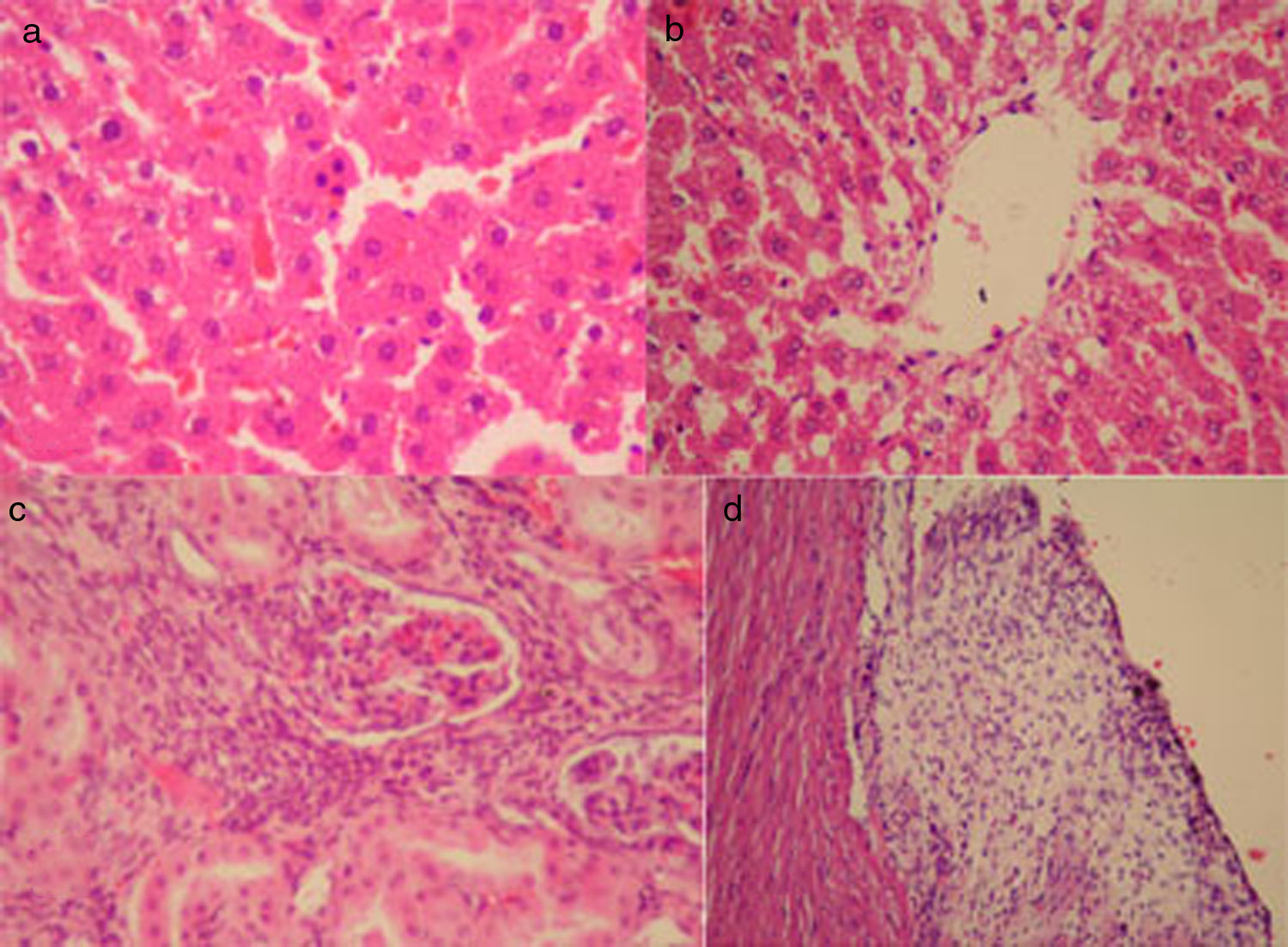
In our study, emphysematous changes were more commonly seen in Group-C (Group-C vs. Group-B; P<.05), (Group-C vs. Group-D; P<.05) (Table 1). In the studies of Yazicioglu et al., emphysematous changes were seldom in the sericin group. However, they used 30mg sericin and did not investigate the effects of 45mg dose. In our study, 45mg sericin resulted in a higher rate of emphysema. On the other hand, fibrin organization and fibrosis in visceral and parietal pleura successfully occurred in all sericin groups more significantly than the sham group (P<.05 between Group-D and each sericin group; Tables 1 and 2). In addition, the Masson's trichrome staining revealed that dense collagen fibers were generated more commonly in sericin groups than the sham group (P<.05 for Group-D vs. each group; Table 3). Finally, multi-layer mesothelium was seen in both visceral and parietal pleura more commonly in Group-B compared to the other sericin groups (Table 2). In the study of Yazicioglu et al., multi-layer mesothelium and mesothelial proliferation were more commonly seen in the sericin and doxycycline groups.16 In the present study, the rate of multi-layer mesothelium in the visceral pleura was 92.3% (n=12) in Group-B and 66.7% (n=8) in Group-C, although the difference was not statistically significant. These findings indicate that the use of sericin at 30mg or 45mg doses leads to multi-layer mesothelium in the visceral pleura and successful pleurodesis (Table 1 and Fig. 4).
As sericin is an intrinsic macromolecular protein, it has a favorable safety profile and does not have significant adverse effects on the lung parenchyma and the other tissues. Therefore, the anticipated adverse effects would be rare according to the relevant literature.15,16,22 However, we suggest that the toxic effects of sericin pleurodesis on the liver should be investigated. In consistent with our findings, Yazicioglu et al. also demonstrated that both pyknotic nuclei and periportal inflammation were more common in the sericin group compared to the silver nitrate and doxycycline groups (P<.05).16 In the present study, sericin administration similarly led to pyknotic nuclei and ballooning degeneration in a dose-dependent manner. While sinusoidal dilatation occurred more commonly in the sericin administrated groups compared to the sham group (P<.05), its rate was similar among the sericin-administrated groups (Table 4).
Glomerular degeneration in the kidney and Pericarditis were seen at a dose-dependent manner (P<.05 for the trend, Table 4). However, glomerular degeneration was not seen and the rate of pericarditis was the lowest in the sericin group in the study of Yazicioglu et al.16 In the present study, glomerular degeneration and pericarditis were seen in four (33.3%) and six (50%) rats in the 45mg sericin group and these rates were significantly higher than the other study groups (P<.05 for each comparison, Table 4). Therefore, we suggest that sericin pleurodesis may lead to nephrotoxicity and pericarditis.
The main limitation of this study is the lack of neurotoxicity evaluation. On the other hand, the pathways and mechanisms of fibrosis associated with sericin pleurodesis are still unknown. Additionally, the fibrosis markers, such as transforming growth factor-β1, basic fibroblastic growth factor, vascular endothelial growth factor, and various other cytokines, must be investigated to validate the effectiveness of sericin pleurodesis. The long-term effects of sericin administration on the thoracic cavity are another relevant research topic. We suggest that sericin may establish a place in routine practice as a novel pleurodesis agent, when its mechanism of action is fully understood, its effectiveness is biochemically demonstrated, its long-term efficacy is established, and the potential allergic or toxic effects are identified.
It is apparent that sericin pleurodesis will be feasible for humans in the near future. It is estimated that the ideal dose in human subjects would be 5–7g. Although no side effects such as pain, fever and irritability, etc. were observed in rats, side effects should be looked for during sericin pleurodesis in human subjects. It is considered that the ideal target patient group would be patients with a malignant pleural effusion in the terminal stage. Following an evaluation of the efficacy of pleurodesis on a case-by-case basis, clinicians should perform further comparative and randomized controlled trials of patient series.
ConclusionsIn conclusion, sericin is a cost-effective macromolecular protein as a result of being a by-product of the textile industry. In addition, it has a low potential for side effects, being a natural product and a high level of efficacy, being a natural glue. Based on our study results, the intrapleural administration of 30mg sericin yields improved results with a high rate of multi-layer mesothelial reaction and a low rate of emphysema and renal and cardiac toxicities, despite a comparable rate of liver toxicities among the groups. We conclude that the optimal sericin dose for pleurodesis in rats is 30mg. However, further well-designed, large-scale, dose-comparison studies are needed to confirm these findings.
Conflict of interestsThe authors declare no conflict of interests.
The authors have special thanks to Prof. Dr. Yahsi Yazicioglu from Gazi University, for statistical analyses.
This abstract has been presented as a poster session in the American Thoracic Society, 2019 Conference, which was held at Dallas, Texas, USA, between 17 and 21 May, 2019.