Papillomas of the respiratory tract are rare epithelial neoplasms. They occur most commonly in children and young adults in the form of multiple lesions located in the upper airway, usually the larynx, sometimes extending to the lower respiratory tract. This type of papillomatosis usually consists of squamous papillomas and is associated with human papilloma virus (HPV) infection.1 Isolated endobronchial papillomatosis, especially the glandular variant, is rare.2 We report the case of an adult patient with glandular endobronchial papillomatosis, limited to the lower respiratory tract, resected by lower right lobectomy via video-assisted thoracoscopy.
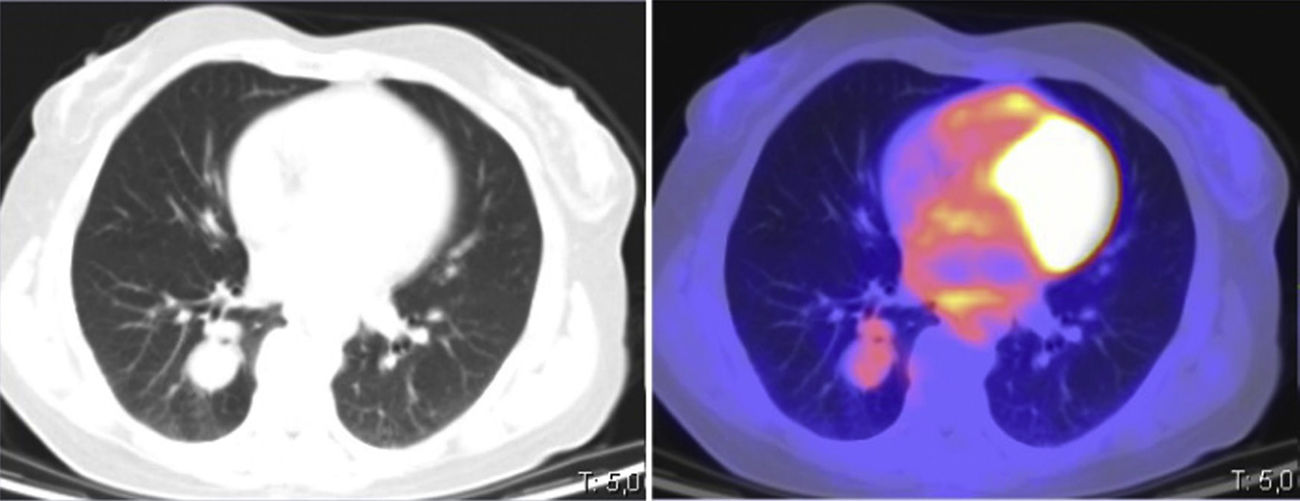
This was a 53-year-old woman, never-smoker with a history of invasive ductal carcinoma of the breast, operated 10 years previously with quadrantectomy and treated with chemotherapy and radiation therapy. The patient was initially examined for a respiratory infection with productive cough associated with wheezing, dyspnea on exertion, and oppressive chest pain. Chest computed tomography (CT) revealed a polylobulated pulmonary nodule in the right parahilar lower lobe measuring 2.1cm, that showed weak to moderate metabolic activity on positron emission tomography (PET-CT) (SUVmax: 2.68) (Fig. 1). Clinical laboratory results and lung function tests were normal. Bronchoscopy showed a pinkish exophytic vascularized mass of soft consistency with necrotic areas that occluded practically the entire basal lobe bronchus, and appeared to originate from an accessory bronchus in the posterior wall.
An incisional biopsy was not diagnostic, with a report of predominantly plasmocytic inflammatory infiltrate. The case was presented to the multidisciplinary committee, and in view of the lack of diagnosis and the impossibility of performing a complete resection by endoscopy, we decided on surgical treatment. In view of the location of the lesion, right lower lobectomy was performed by videothoracocopy. The postoperative course was favorable and the patient was discharged after 4 days.
The final diagnosis was endobronchial papillomatosis, with three glandular papillary lesions, the largest measuring 2.5×1.6cm, along with two millimetric lesions, one of which occurred in continuity with the larger one. The lesions extended from the lobar bronchus to the bronchioles. Histological changes consisted of papillomatous proliferations with a respiratory-type epithelial lining, mucosecretory cell hyperplasia, squamous metaplasia, and cuboidal cells. Of note in the stroma was the presence of a lymphoplasmocytic infiltrate, and foamy histiocytes. No cell atypia was detected, and mitosis was scant.
The patient has continued to attend periodic check-ups with follow-up CT and bronchoscopy, and has shown no signs of recurrence after 18 months.
Respiratory tract papillomas consist of rare epithelial neoplasms that may be classified according to the number of lesions, location, and histology.2 The lesions may present in multiple forms, and generally appear in the upper respiratory tract, although they may affect any point of the airway, extending to the lower respiratory tract in up to 30% of cases.3 They tend to recur, hence the name “recurrent respiratory papillomatosis”.4 This is the most common form in children and young people, although an adult form with similar characteristics has been described.5 It is caused by HPV, mainly serotypes HPV-6 and HPV-11. Treatment is based on the resection of lesions usually with laser, combined with antiviral drugs.6
The isolated form is less frequent, although the actual incidence is unknown. This is the most common form of presentation in adults, occurring usually in the fifth or sixth decade of life with a greater incidence in men.7 It usually presents as a polypoid nodule in the trachea, or the lobar or segmental bronchus. We can differentiate between central or peripheral papillomas, depending on site, and this will also affect the form of clinical presentation. The most common symptom of endobronchial papillomas is cough, which may lead to atelectasis and postobstructive infections. Other possible symptoms are fever, hemoptysis, and dyspneai. Peripheral papillomas are usually asymptomatic and discovered incidentally.2
Three histological forms have been described: squamous, glandular, and mixed. The squamous variant is the most common, and is believed to be caused by HPV.8 This type has been associated with a potential risk of malignant transformation, which ranges between 8% and 40%, depending on the series.9 This risk increases with exposure to tobacco10; moreover, the serotypes HPV-16 and HPV-18 are associated with a higher risk of malignant transformation.11,12
The glandular variant is less common. In the largest series published in the literature, Tryfon et al.11 described 32 cases of lower airway papillomas, of which only 6 were glandular. This article also includes a review of published cases, and of a total of 69 cases, only 14 were glandular. It is generally thought to affect older patients, is unassociated with smoking, and usually occurs in a peripheral location. Malignant transformation of glandular papilloma has not been described.13
As for differential diagnosis on pathology examination, it can be sometimes difficult to distinguish between the secondary changes that can appear in these lesions suggesting possible malignant transformation and a false impression of interstitial microinvasion or focal changes suggestive of adenocarcinoma with lepidic pattern, in cases of glandular or mixed papilloma.14,15
Treatment consists of resection; the method of choice will depend on the size, location, and preoperative diagnosis. Small endobronchial lesions can be treated endoscopically, while larger or peripheral regions will require surgical resection. In most published cases, treatment was surgical, including subsegmental resections, lobectomies, and even pneumonectomies.11,15
In our case, we could not reach a preoperative diagnosis. Given the location and the broad base of implantation, we decided to perform surgical resection, revealing a final diagnosis of glandular endobronchial papillomatosis.
In summary, endobronchial papillomas are lesions that, despite their low incidence, must be taken into account in the differential diagnosis of lung nodules in adults. The glandular variant is the most uncommon, prognosis is good, and results after surgical resection are excellent.
Please cite this article as: Bayarri Lara CI, Moyano Rodríguez MJ, Torres Bermúdez JR, Ruiz Zafra FJ. Resección quirúrgica de papilomatosis glandular endobronquial. Arch Bronconeumol. 2019;55:278–279.