Spirometry is usually the first lung function test performed during the clinical assessment of respiratory diseases.
The bronchodilation test (BDT) consists of comparing the spirometric variables before and after the protocolized administration of a short-acting β2-adrenergic agonist (SABA).1
The study of bronchial reversibility is indicated for: (a) obtaining an obstructive spirometry for the first time; (b) evaluating the possible response to additional treatment or alternative therapeutic regimens in patients with known reversibility and whose forced expiratory volume in 1 second (FEV1) remains below 80% predicted despite treatment; (c) determining the degree of impairment; (d) evaluating airflow limitation in a preoperative situation,1,2 and (e) when asthma is suspected, measuring airflow limitation, determining reversibility, and confirming the diagnosis.1,3
To ensure quality, the BDT must be performed using the right instrument, technique, bronchodilator, dose, and timing, and it must be administered by competent, trained staff.1
SEPAR rules recommend the use of SABA (400μg [4 puffs of 100μg] at 30-second intervals) or ipratropium bromide (total dose of 160μg). In both cases, it is preferable to use pressurized cartridges with a spacer and a proper technique. Terbutaline can be used as an alternative to salbutamol.1 The minimum time between spirometric maneuvers must be 15min after inhalation of salbutamol or 30min after ipratropium bromide.1
BDT is considered positive when it meets at least one of the following criteria: an improvement in FEV1 or forced vital capacity (FVC) of at least 12% and ≥200ml in the post-bronchodilator spirometry results compared to baseline spirometry values.1
Because this test is susceptible to many variable conditions, studies have been performed to explore whether pulmonary reversibility can be affected by the drug used and the underlying disease of the patient. Gross, in a study of patients with asthma and COPD,4 observed that the bronchodilator effect of SABA is greater in asthmatics. However, in COPD patients, ipratropium bromide has proved to be more effective.4,5
Other studies have shown that the effect of the drug administered is the same, regardless of the type of device (pressurized cartridge, spacer, or dry powder),6 although to standardize the BDT, the best option (according to SEPAR, mentioned above) is to use pressurized cartridges with a spacer and a proper technique.
Aware of the degree of variability in the conduct of BDTs in clinical practice, we wondered if the human factor had been studied closely enough, in terms of experience, expertise, and technical skills, as these are essential considerations that affect the results and the quality achieved by professionals performing these tests.7
This study was motivated by the absence of studies that explore the characteristics of the professionals who perform this test and how it is administered. The objective was to determine the work setting in which nurses perform this test, to determine their experience, and to describe the drugs, dosage, waiting time, and method of administration in BDT.
We performed a descriptive, cross-sectional, multicenter, 2-phase study. In the first phase, a measuring instrument was designed and validated to meet the objectives described above (Delphi technique and confirmatory factor analysis). In the second phase, we distributed this tool via an online questionnaire to nursing professionals from different health centers in the Community of Madrid working in lung function laboratories (46%), outpatient clinics (25%), primary care (16%), hospitals (7%), specialized care (4%), and occupational risk prevention centers (2%). The study was conducted between 2015 and 2017.
A total of 63 completed surveys were received, of which 5 were discarded after comparison of different variables showed that they may have been duplicates.
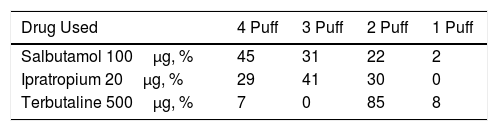
We found discrepancies among the respondents with regard to the type and dose of drug used (Table 1).
In total, 86% of professionals used a spacer and pressurized inhaler for the administration of the drug, 12% administered the bronchodilator without a spacer, and only 2% used both forms interchangeably.
With regard to performing the spirometry, 55% of nurses waited 15min, 35% waited 20min, and the remaining 10% waited 10, 30 or 12min.
Eighty-six percent of nurses believed that they knew how to interpret the BDT and 97% had been performing the test for at least 1 year.
In view of these results, we can conclude that, in spite of the consensus with regard to the technique and interpretation of the BDT, the reality is that administration techniques vary among professionals who perform these tests, and these factors may affect pulmonary reversibility.
We conclude that it is important to control factors that can influence the administration of the BDT (technique, training and knowledge of the administering practitioner, the drug used, etc.) because they can impact on lung reversibility.
It would be advisable to carry out training programs to increase the quality and reproducibility of tests carried out by nursing professionals, aimed at standardizing criteria and minimizing human errors.
Please cite this article as: Enríquez-Jiménez M, Arranz-Alonso S, Frías-Moreno A, Batanero-Rodríguez A. ¿Cómo realiza enfermería la prueba de broncodilatación?: estudio multicéntrico en la Comunidad de Madrid. Arch Bronconeumol. 2019;55:280–281.