Mediastinal fibrosis (MF) is one of the most common non-malignant causes of superior vena cava syndrome (SVCS), along with thrombi forming on intravascular devices (central lines, pacemaker cables, etc.). However, the most common cause of SVCS remains malignant disease, particularly lung cancer. In endemic regions, MF is a relatively common complication of infections caused by Histoplasma capsulatum, although it is more common in our setting to find idiopathic forms, forms associated with immunoglobulin (Ig) G4 deposition (in the context of IgG4-related diseases, such as retroperitoneal fibrosis or Riedel's fibrosing thyroiditis), or forms caused by other granulomatous diseases, such as tuberculosis.1–4
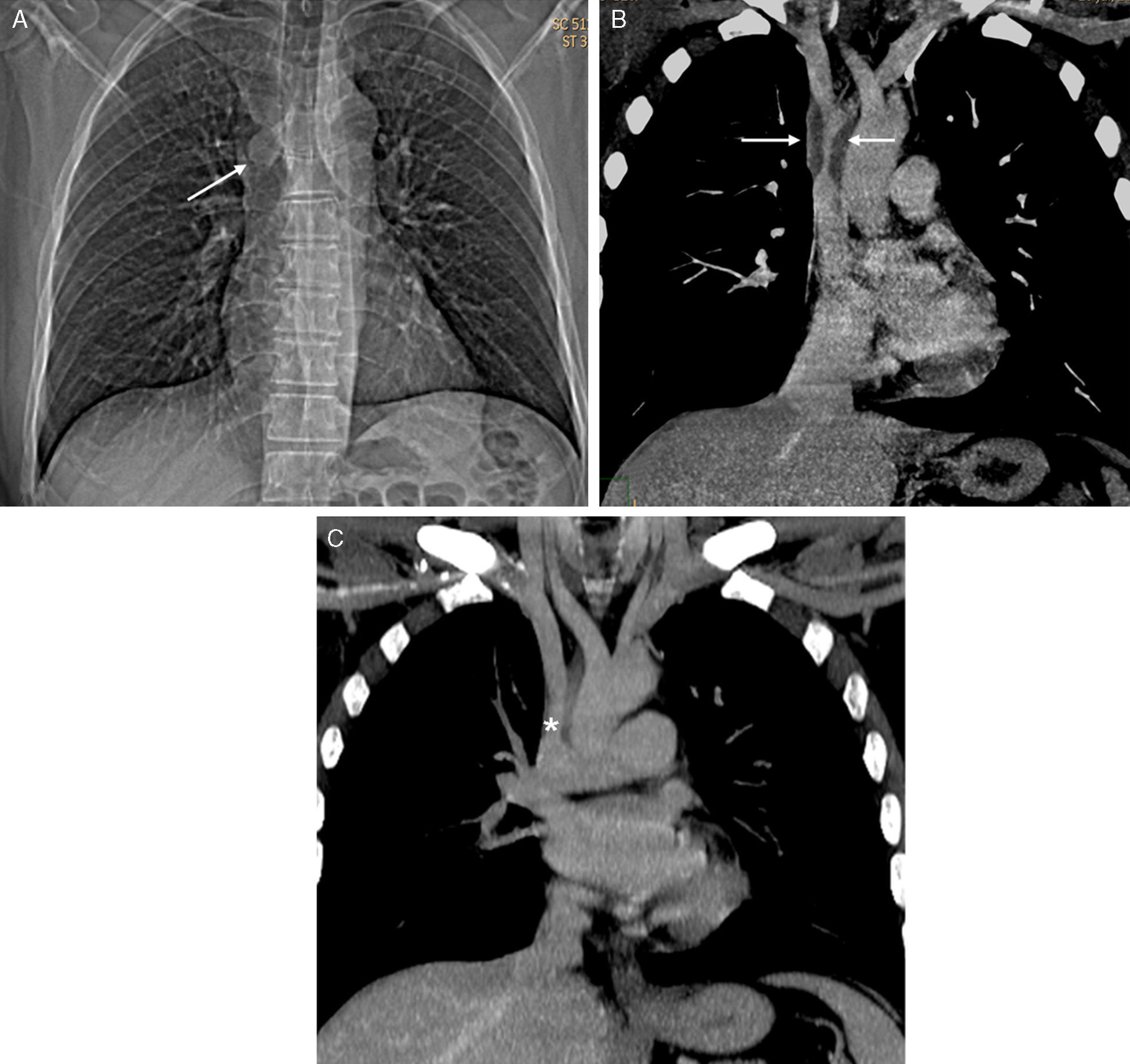
We report the case of a 44-year-old man, non-smoker, who presented in our hospital with a 1-month history of progressive clinical symptoms of headache and edema of the face and upper limbs. Chest X-ray showed slight widening of the right paratracheal stripe (Fig. 1A), but no parenchymal opacities or pleural effusion. On physical examination, dilation of the neck veins and edema of the face and cervical spine were the only observations of note. Chest computed tomography (CT) confirmed a soft tissue mass that surrounded the circumference of the upper SVC causing severe stenosis of the lumen (Fig. 1B). No radiological signs of previous tuberculosis infection and no infiltration of other mediastinal or lung structures were observed. Tuberculin testing was negative and the patient had never visited any country in America. IgG4 serum levels were normal. A diagnosis of a localized form of MF was proposed, and confirmed with mediastinoscopy. Histology study revealed a fibrous tissue with chronic inflammatory cell aggregation and abundant collagen bundles, with no signs of vasculitis or granulomas. Biopsy culture was negative for fungi and mycobacteria. The patient was initially treated with systemic corticosteroids and anticoagulants, with progressive clinical improvement. A repeat follow-up CT at 4 weeks (Fig. 1C) showed radiological improvement of the SVC stenosis, so after consultation with the Departments of Thoracic Surgery and Vascular Radiology, need for stent placement or bypass was ruled out.
(A) Chest X-ray showing subtle widening of the paratracheal stripe (arrow). Neither parenchymal opacities nor pleural effusion is observed. (B) Coronal maximum intensity projection (MIP) reconstruction confirming a soft tissue mass surrounding the circumference of the SVC, causing severe stenosis of its lumen (arrows). Coronal MIP reconstruction carried out 4 weeks after starting treatment, showing improvement in SVC stenosis (asterisk).
In our opinion, this case is interesting because it illustrates the importance of imaging studies in the diagnosis, staging and follow-up of an SVCS caused by an idiopathic localized form of MF exclusively affecting the SVC.
Please cite this article as: Gorospe Sarasúa L, Picón Serrano C, Muñoz Molina GM. Síndrome de vena cava superior secundario a una forma focal idiopática de fibrosis mediastínica. Arch Bronconeumol. 2016;52:53–55.