Chylothorax is defined as the presence of triglycerides in pleural fluid (>110mg/dl) with a pleural fluid/serum ratio >1, positive Sudan III staining or detection of chylomicrons. It is the most common cause of pleural effusion in fetuses and neonates, but in adults it accounts for only 3% of cases of this entity. It is mainly caused by cancer (lymphoma in 75% of cases), followed by iatrogenesis and injury. Other rare causes include lymphangiomyomatosis, sarcoidosis, tuberculosis, congenital and idiopathic lymphatic malformations.1
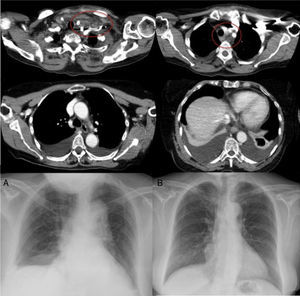
We report the case of a 60-year-old patient with a history of arterial hypertension, dyslipidemia, and hypothyroidism receiving medical treatment. After a violent sneeze, she developed left supraclavicular swelling and dizziness, which prompted her to visit the emergency room. The chest radiograph revealed bilateral basal pleural effusion; cervical-chest computed tomography (CT) showed left laterocervical-supraclavicular collection extending to all mediastinal compartments, with bilateral pleural effusion (Fig. 1), interpreted by the radiologist as hematoma following a violent sneeze. A wait-and-see approach was adopted, and after bilateral progression of the effusion was confirmed on X-ray, endopleural drainage tubes were placed in both sides. Fluid with a chylous appearance was obtained from both hemithoraces, and analysis of samples from both sides confirmed sterile exudate with a high triglyceride concentration (2241mg/dl in the right hemithorax and 2160mg/dl in the left). After diagnostic confirmation of bilateral chylothorax, dietary treatment was initiated, with restricted fat intake. Fluid collected from both drainage tubes reduced progressively, becoming serous in appearance after the introduction of dietary restrictions, confirming the biochemical resolution of the chylothorax. In view of the patient's favorable progress, no other therapeutic measures were introduced, and the pleural drainage tubes were removed from the left side after 48h (Fig. 1A) and from the right side after 5 days. After removal of the drainage tubes, radiological monitoring confirmed bilateral resolution of the effusion. Resolution of clinical and radiological signs and symptoms were confirmed in outpatient follow-up (Fig. 1B).
Axial computed tomography slices showing left laterocervical-supraclavicular collection, with diffuse extension throughout all mediastinal compartments (circled) and bilateral pleural effusion. (A) Posteroanterior radiograph of chest after removal of left pleural drainage tube, with the right pleural drainage tube still in place. (B) Posteroanterior radiograph of chest during follow-up, 3 months after the episode, showing complete resolution of bilateral pleural effusion.
Minor injury triggering chylothorax has been described in the literature: forced stretching of the upper limbs, or maneuvers that increase intrathoracic pressure, including vomiting, hiccoughs after ingestion of high-fat foods, cough, childbirth or, very rarely, sneezing – as in our case. We found no other case of chylothorax caused by sneezing in either PubMed or Embase.1,2 Cases in which no cause of disruption of the thoracic duct can be determined on examination are considered spontaneous; however, concomitant presence of a fragile duct is very likely to be a predisposing factor.2 Very few cases have been reported in the literature; a review of similar cases reveals a rather well-defined pattern, consisting of the appearance of left supraclavicular swelling along with bilateral chylothorax after mild exertion in a woman in her fifth decade of life.3 In our patient, the temporal relationship between the sneeze and the appearance of lymphatic effusion in the absence of any other specific cause led us to establish a diagnosis of spontaneous chylothorax. Performing a CT is important for the correct characterization of the clinical picture and the grade of involvement, and for detecting any underlying issue (thoracic duct disease, lymphadenopathy, masses, lung disease, etc.).4,5 Unlike cases caused by major traumatism, rupture of the thoracic tract is minimal in spontaneous cases and lymphography is generally inconclusive; it is unlikely that further studies other than CT and analysis of the pleural fluid, such as we performed in our case, will be required.
In general, the best treatment for chylothorax is to correct the underlying cause when it is identified.1 Therapeutic management may include conservative measures (dietary restriction of fats, evacuating thoracocentesis, parenteral nutrition, treatment with octreotide), minimally invasive measures (pleural drainage, pleurodesis, interventional radiological techniques), and surgical intervention (thoracic duct ligation with video-assisted thoracoscopy or thoracotomy).5 When the amount of fluid collected is sparse, as in spontaneous cases, chylothorax can be appropriately controlled with dietary treatment and evacuation of pleural effusion, if demanded by the volume, with evacuating thoracocentesis or pleural drainage,2,3 as in our case. It is important for physicians to understand spontaneous chylothorax, as prognosis with conservative treatment is good, in contrast to chylothorax induced by other causes.
Please cite this article as: García-Tirado J, Landa-Oviedo HS, Suazo-Guevara I. Quilotórax espontáneo bilateral desencadenado por estornudo: una entidad peculiar de buen pronóstico. Arch Bronconeumol. 2017;53:32–33.