Lung cancer is a neoplasm with high mortality, responsible for more than 20% of deaths per year in European countries.1 It is the most frequent cause of cancer death in western men, with a 5-year survival of 7.9%.2 Sarcomatoid tumors account for only 0.3%–1.3% of lung cancers, with an even lower prevalence of pleomorphic carcinoma.3
Lung cancer metastases to the digestive tract are rare, with an incidence varying from 2% to 14% in some autopsy series.4 These metastases normally do not become apparent until complications such as bleeding, bowel obstruction, or perforation occur. Once this happens, the prognosis and survival worsen. We present the case of a 71-year-old man, a former smoker of 100 pack-years up to 5 years ago, with a history of hypertension, diabetes and chronic obstructive pulmonary disease, who underwent emergency surgery for symptoms of bowel obstruction in the postoperative period following lung resection for suspected cT4N0M0 lung cancer. He presented a complete study carried out 6–8 weeks prior to the surgery: fibrobronchoscopy, functional tests, chest-abdominal computed tomography (CT) and positron emission tomography (PET)/CT, where a nodule was found in the left upper lobe (LUL) and another in the left lower lobe (LLL), with no evidence of extrathoracic disease. Endobronchial ultrasound (EBUS) was negative for malignancy. Left lower lobectomy and atypical resection of the nodule were performed in the LUL by video-assisted thoracoscopic surgery (VATS), accompanied by lymphadenectomy of the hilar regions5–7 and pulmonary ligament.
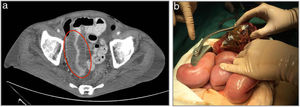
On postoperative day 4, the patient presented symptoms of intestinal obstruction. Urgent abdominal CT revealed a perforated obstructive mass at the level of the ileum (Fig. 1A) requiring emergency surgery, where we found peritonitis located in the right iliac fossa and intussusception caused by a 12-cm perforated necrotic mass located in the terminal ileum (Fig. 1B). Numerous reactive adenopathies were also found in the adjacent mesoileum, requiring peritoneal lavage, tumor resection and ileal anastomosis for transit reconstruction. Postoperative recovery was uneventful, and the patient was discharged on postoperative day 7. Histopathological analysis of the abdominal tumor confirmed the diagnosis of a 12-cm pleomorphic lung cancer metastasis (pT2bN0M1b).
Finally, after histological analysis of the lung lesions, it was concluded that they were 2 synchronous tumors: LUL squamous cell carcinoma (pT1bN0) and LLL giant cell pleomorphic carcinoma (pT2bN0M1b). McNeill et al. and Berger et al. conducted studies with a total of 1975 lung cancer patients, where only 0.5% and 0.1%, respectively, showed intestinal symptoms due to metastases.4,5 Studies such as the one by Ito et al. based on the behavior of pleomorphic lung carcinoma in 22 patients showed metastases in up to 10 of them (45%) in the course of follow-up.6
Bowel metastases should be considered in the differential diagnosis of patients with lung cancer and gastrointestinal symptoms, with a higher degree of suspicion in cases of pleomorphic carcinoma.
Urgent surgical treatment seeks to improve prognosis and short-term survival.
The interest of this case lies not only in the diagnosis of the intestinal metastasis itself, but in the false negative of the extension study—completed 6 weeks before the surgery—that unusually did not show the abdominal lesion, which would have changed the initial therapeutic strategy. This could be attributed to the aggressiveness described in this histological lineage.7,8
Please cite this article as: Varela Recio J, Camacho Marente V, Triviño Ramirez A, Espinosa Jimenez D, Pacheco Garcia JM. Metástasis de carcinoma pulmonar pleomórfico como causa de abdomen agudo. Arch Bronconeumol. 2020;56:334–335.