We read with great interest the original article by de Gregorio et al.,1 who analyzed success in vena cava filter (VCF) retrieval and factors associated with retrieval failure. They also commented on complications associated with VCF placement and removal, especially those of a local nature (tilting of the inferior vena cava axis, venous wall penetration, migration, and local thrombosis). We would like to highlight another important complication related to VCF use that is of interest to pulmonologists: filter embolization.
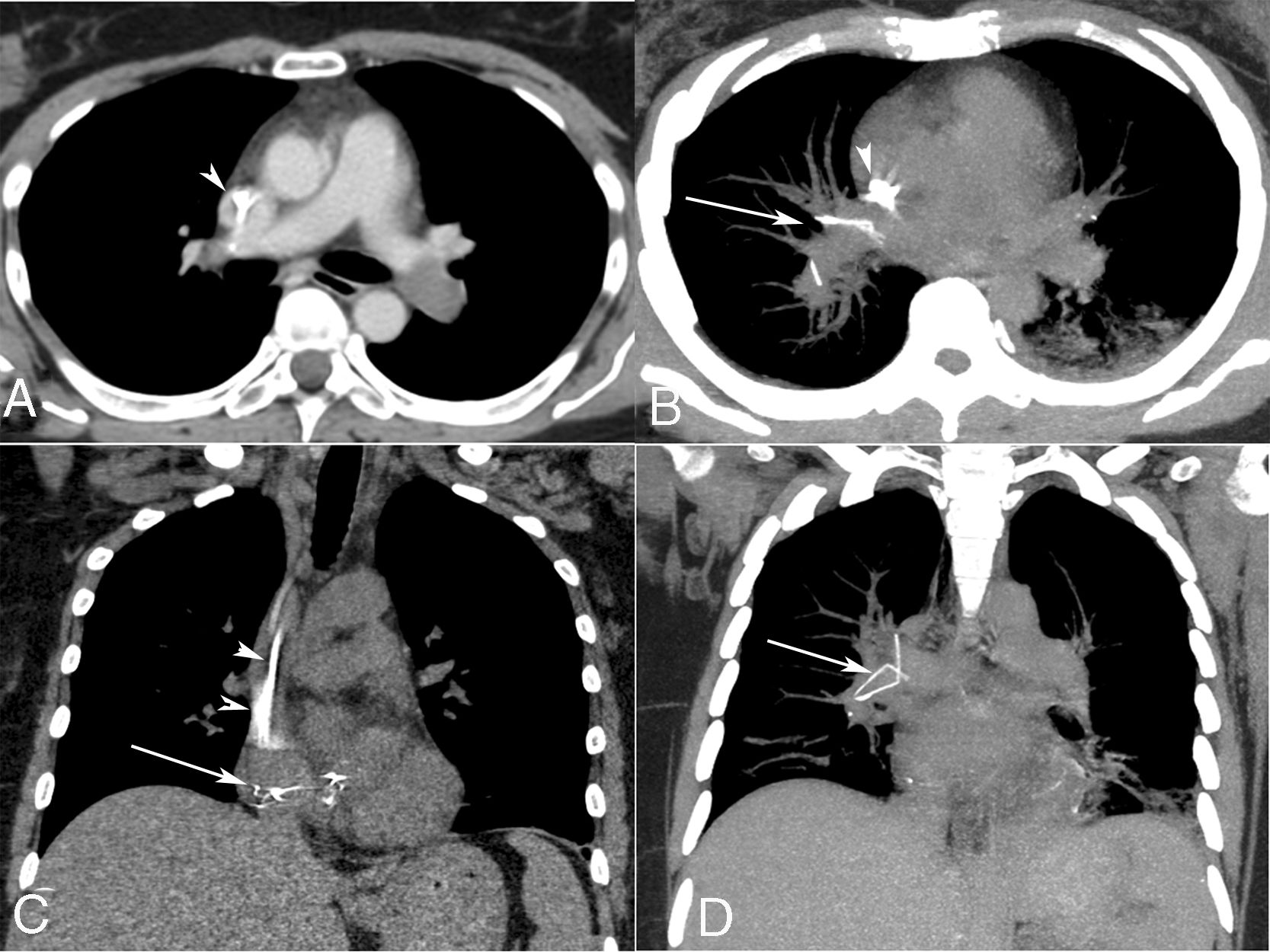
A 47-year-old woman presented to the emergency department with acute shortness of breath and chest pain. She had a past history of recurrent deep venous thrombosis, despite anticoagulation therapy. A VCF had been inserted in the infrarenal inferior vena cava 9 months previously. Computed tomography of the chest identified a thrombus in the left pulmonary artery with pulmonary opacities in the left lower lobe, and multiple metallic fragments at the level of the right pulmonary artery and right atrium (Fig. 1). The diagnosis of pulmonary infarction and embolization of a broken VCF was made. Given the patient's relatively young age and the possibility of future complications, the patient decided to have the fragments surgically removed. The patient recovered well and was discharged 2 weeks after surgery.
Axial (A) contrast-enhanced chest computed tomography image showing a filling defect (thrombus) on the left pulmonary artery. Axial (B) and coronal (C and D) reformatted images with maximum intensity projection show multiple metallic fragments (from the fractured filter) at the level of the right cardiac cavities and right pulmonary artery (arrows). Note also non-homogeneous opacities in the left lower lobe (pulmonary infarction) and a deep venous catheter in the superior vena cava (arrowheads).
VCF complications can occur early, during placement, or later, after positioning. Immediate complications of VCF placement include puncture site complications and mechanical failures, such as delivery system malfunction, incomplete or asymmetric deployment (opening), malpositioning, and tilting. Fatalities caused by these complications are rare.2,3
Late complications of VCF use may be of local origin, including inferior vena cava thrombosis, penetration of the vessel wall and injury to nearby organs, or distant, including structural failure with migration of all or part of the VCF to the right side of the heart and/or pulmonary arteries, recurrence of thrombosis and pulmonary embolism.2,3 Distant complications are of special interest to pulmonologists.
Filter fracture occurs when the filter structure fails, leading to fragmentation and potential embolization of the fragment. Filter embolization is defined as movement of the filter after deployment to a distant anatomic site completely out of the target zone. The most common site of embolization is the right atrium, where the fragment can cause complications such as perforation of the right atrial wall, cardiac tamponade, and myocardial infarction. Another common site is the pulmonary vasculature.3,4
The proper management of patients with intracardiac or intrapulmonary VCF migration remains speculative. Serious consideration should be given to filter removal whenever possible, regardless of the presence or absence of symptoms. Surgery should be the first option considered. Open thoracotomy has the advantage of allowing the operator to directly visualize the filter and have better control during retrieval. It also allows direct inspection of the cardiac chambers and immediate repair of any damage that has occurred. Whenever surgery is contraindicated, endovascular retrieval should be performed by an experienced endovascular team.4,5