The criteria for home oxygen therapy (HOT), proposed more than 20 years ago, establish that patients with COPD who are non-smokers, correctly follow treatment and present respiratory failure in a context of clinical stability should receive HOT. Specifically, those patients with PaO2<55mmHg or those with PaO2 between 55 and 60mmHg in whom there are signs of repercussions in the organs from hypoxemia, such as pulmonary hypertension, chronic cor pulmonale, congestive heart failure, heart rate disorders or polycythemia (hematocrit>55%), or those with lower intellect, would be ideal candidates. In this group of patients, HOT has demonstrated its benefits in terms of survival and improvement of the clinical parameters.1
These universally-accepted criteria are valid at sea level. However, many of our patients do not live at sea level, and one must contemplate whether these criteria are equally applicable at other altitudes. Studies have been done to estimate the degree of hypoxemia that a patient can reach when moved to a certain altitude, basically aimed at evaluating the need for the administration of oxygen (O2) during airplane travel.2,3 However, the prediction equations of a certain level of PaO2 that are based on a baseline PaO2 value obtained at sea level cannot be applied inversely. We cannot estimate the PaO2 that a patient would have at sea level by using his/her PaO2 determined at a certain altitude.
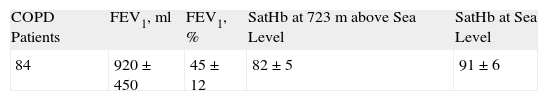
Our group has worked with patients residing in Madrid at an altitude of 723m with criteria for respiratory failure whose arterial saturation has ostensibly improved at sea level. That is to say that patients with criteria for HOT in Madrid may no longer meet said criteria when the altitude effect is cancelled out (Table 1). Many of these patients would not receive HOT if they lived at sea level, which leads us to suppose that there is an excess of indications for HOT in Madrid simply due to the altitude effect. A somewhat similar situation has been demonstrated in critical patients with regards to the PaO2/FiO2 ratio. Pérez Padilla4 has clearly observed that the patients have a lower shunt and presumably a lower degree of lung injury than residents at sea level when meeting the criteria for progressive adult respiratory distress syndrome with a PaO2/FiO2 ratio of 200mmHg. This author suggests keeping in mind the effect of altitude when comparing these patients in published studies as there can be important differences in the results obtained.
The effect of acclimatization or adaptation to heights of humans is well known. There are two fundamental mechanisms developed by subjects living at moderate altitudes, these being the increase in ventilation and the decrease in plasma volume, with consequent hemoconcentration.5 The increase in red blood cells maintains the total oxygen content of the blood and guarantees the transport of oxygen to the tissue. What is attractive is the hypothesis that the absolute PaO2 value in a COPD patient would not be the best indicator for whether to receive home oxygen therapy. Instead, the degree of efficacy of the compensatory mechanisms of the patient and his/her degree of adaptation to the altitude in which he/she lives would be a better indication. It is necessary to develop studies that more thoroughly analyze these physiological adaptation mechanisms in order to establish dynamic criteria for considering HOT. Currently, HOT is prescribed by extrapolating the criteria established at sea level to the entire population. Thomas Petty said on an occasion: “If we applied the HOT criteria in Denver (Colorado – 1,609m above sea level), we would have to give O2 to the entire population”.6 Does this make sense? We should reconsider HOT criteria according to altitude.
Please cite this article as: Díaz-Lobato S, Mayoralas Alises S. ¿Deberíamos reconsiderar los criterios de oxigenoterapia crónica domiciliaria en función de la altitud? Arch Bronconeumol. 2011;47:421–2.