All workers exposed to cereal flours (not only bakers), may develop sensitization and occupational rhinoconjunctivitis and/or asthma in response to cereal flour allergens.1,2
We report the case of a 31-year-old woman, employee in a furniture factory for nine years, with a history of mild allergic rhinoconjunctivitis and asthma due to house dust mites. She reported a 3-year history of work-related rhinoconjunctivitis. Two years before referral to our clinic she began to have dry cough and breathlessness, which she also attributed to her work environment. All these symptoms increased minutes after handling rye flour, a component of the wood glue used for building furniture.
Skin prick tests (SPT) were positive for grass and olive pollens, Dermatophagoides pteronyssinus, wheat flour and rye flour. SPT using a specially prepared extract of wheat flour and rye flour (10%, wt/vol) were strongly positive (papules measuring 10 and 12mm respectively). Specific IgE (ImmunoCAP, ThermoFisher, Uppsala) was 4kU/L for rye flour, 2.6kU/L for D. pteronyssinus, and 2.1kU/L for wheat flour.
Spirometry performed when the patient was at work showed FEV1 2.40L (82%) and FEV1/FVC 80%. A methacholine inhalation challenge test also performed in the workplace following an abbreviated protocol3 was positive (0.21mg cumulative dose).
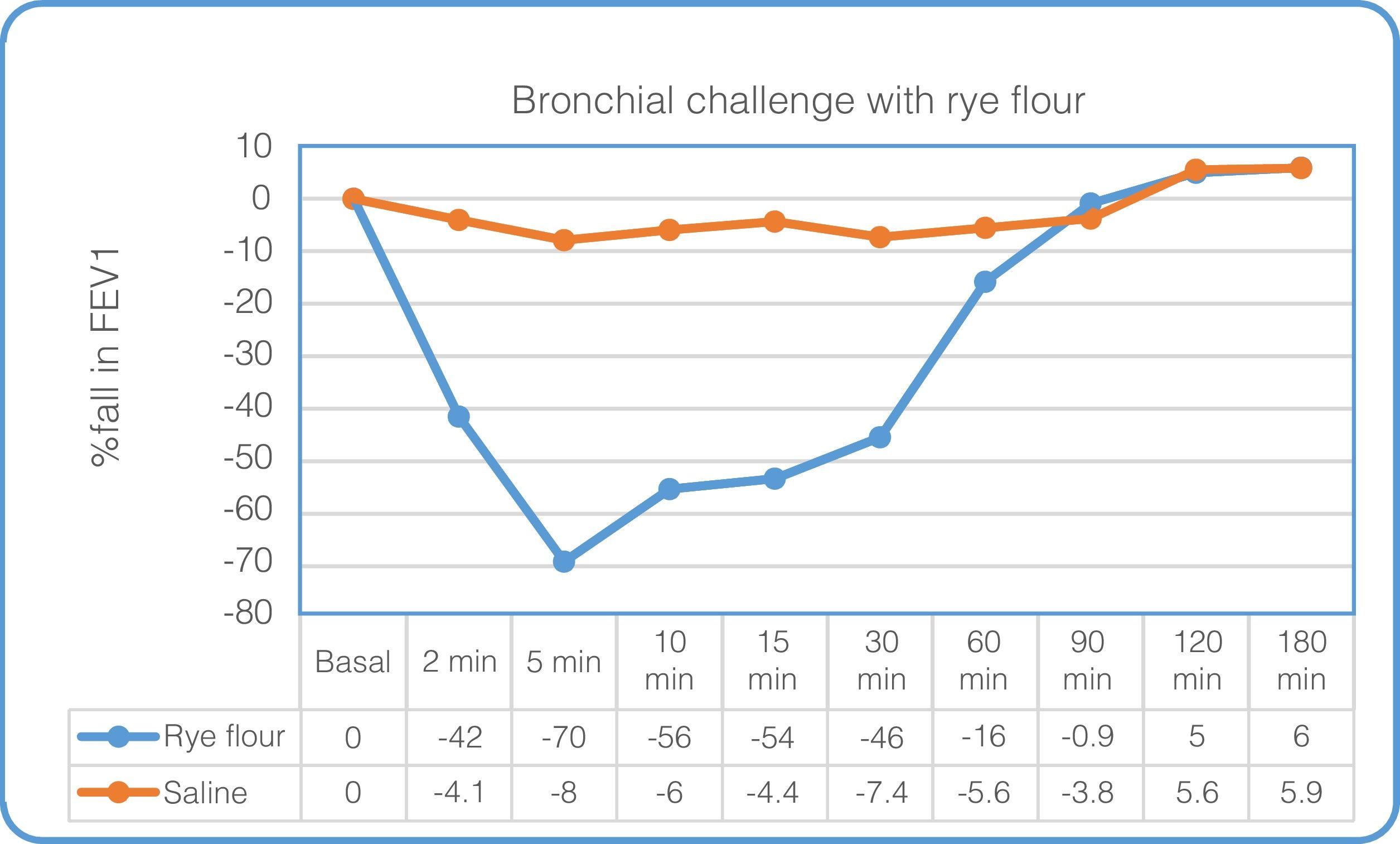
A specific inhalation challenge test was carried out in the hospital lab by tipping rye flour from one tray to another, increasing the duration of exposure to a maximum of 15min. Spirometry was performed at baseline, after each exposure and at 2, 5, 10, 15, 20, 30, 45, 60, 90, and 180min after the challenge with rye flour. Peak expiratory flow was then measured hourly over 24h (except during sleep). Exposure to rye flour was interrupted after the 2min challenge because of cough and dyspnea. A 70% fall in FEV1 with respect to baseline values was observed at 5min (Fig. 1). A control challenge with normal saline was performed 1 day before the inhalation challenge and no significant changes were observed.
DiscussionOur patient's respiratory symptoms were work-related; her disease course, together with the results of diagnostic tests, indicated an occupational allergic respiratory disease triggered by IgE-mediated allergy to inhaled rye flour.
Rye flour allergens should be considered in the diagnosis of occupational asthma in bakers, farmers, and millers.4 However, the task performed in the workplace must also be taken into account, because, while some jobs are not generally associated with occupational exposure to flour, these substances can be used in certain circumstances for specific tasks, as in the reported case.1
Workers at risk of sensitization are those who are atopic and whose tasks include sieving and mixing ingredients, as occurred in our patient.1 She also showed very high specific bronchial hyperreactivity, similar to that found by other authors reporting rye flour allergy.5
We describe a rare case of occupational rhinoconjunctivitis and asthma caused by rye flour in a furniture factory worker, a job not usually associated with occupational respiratory disease caused by cereal flours.
Please cite this article as: Gómez-Torrijos E, Núñez M, Rodríguez RG. Rinoconjuntivitis y asma ocupacional en una trabajadora de una fábrica de muebles. Arch Bronconeumol. 2016;52:227–228.