Buckwheat or saracen (Fagopyrum esculentum) is a herbaceous plant of the Polygonaceae family, native to Central Asia. It has a high nutritional value, with a higher protein and fatty acid content than cereals.1,2 Cases of IgE-mediated buckwheat allergy have been reported, caused by both inhalation of flour and ingestion. It presents with rhinoconjunctival, bronchial, gastrointestinal, and cutaneous symptoms, and even anaphylaxis.3–5 We report a case of rhinoconjunctivitis and occupational asthma due to buckwheat flour allergy in a baker.
Our patient was a 45-year-old man with a history of allergic rhinitis due to dust mite sensitization who had been a baker for 26 years. He consulted due to an 8-month history of episodes of cough, dyspnea, sneezing, watery rhinorrhea, nasal congestion, and ocular pruritus, occurring exclusively in the workplace on the days that his colleague was kneading dough with buckwheat flour. His symptoms remitted at home.
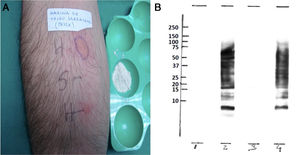
On physical examination, the patient had bilateral nasal obstruction and was in good general condition, afebrile and eupneic, with normal cardiopulmonary auscultation. The allergy work-up began with skin tests (prick test) with battery of airborne allergens and foods (commercial extracts) including wheat flour, barley, rye, oats, maize, rice, gliadin, nuts, milk, egg and lipid-carrying proteins. Results were positive for dust mites and 5% P/V buckwheat flour extract (9mm×7mm). In addition, prick-to-prick tests were performed with an extract of buckwheat prepared by us from flour provided by the patient, which gave a positive result (18mm×11mm) (Fig. 1). The study was then extended by determining IgE using the ImmunoCAP method™ (purified extract) with the following results: total IgE 187KU/l, specific IgE for buckwheat 15.4KU/l, wheat and rye <0.1KU/l, Dermatophagoides pteronyssinus 10.1KU/l, and Lepidoglyphus destructor 1.98KU/l.
(A) Prick-to-prick with buckwheat flour. (B) IgE-immunodetection of buckwheat flour extracts. 1: buckwheat (non-reducing conditions)+negative control. 2: buckwheat (non-reducing conditions)+patient serum. 3: buckwheat (reducing conditions)+negative control. Buckwheat (non-reducing conditions)+patient. On the left, position of the molecular weight markers (10, 15, 20, 25, 37, 50, 75, 100, 150, 250kDa).
Chest X-ray showed no pathological changes. Spirometry was normal: forced vital capacity (FVC) 6060ml (115%), forced expiratory volume in 1s (FEV1) 4820ml (113.5%), FEV1/FVC (80.63%), with a negative bronchodilator test, and FeNO of 115 parts per billion. The nonspecific bronchial challenge test with methacholine performed while the patient was still working was positive (0.022mg).
In view of the findings described, we decided to perform a specific bronchial challenge test (SBCT) while he was on sick leave. Initially there was no variability after exposure to placebo. Four minutes after the first exposure to the allergen in the cabin using a mixture of lactose and buckwheat flour, acquired externally, at low concentration, using the method described by Pepys, the patient presented severe bronchospasm with a 35% fall in FEV1 from baseline.
Finally, in order to identify the specific proteins of the buckwheat that induced IgE antibody synthesis in this patient, immunoblotting was performed, using the same extract made from the flour provided by the patient. Several IgE binding bands against different extract proteins were detected in reducing and non-reducing conditions (from <9 to 75kDa) (Fig. 1).
Although we could not rule out the presence of mites in the extract used for skin tests, immunoblotting and SBCT, the determination of specific IgE by ImmunoCAP™ confirmed sensitization to buckwheat flour.
The patient was diagnosed with IgE-mediated occupational rhinoconjunctivitis and asthma due to buckwheat flour allergy. He was advised to avoid exposure to this flour and to start treatment with long-acting bronchodilators and inhaled corticosteroids to avoid progression and chronification of symptoms.
Buckwheat, despite its name, has no taxonomic relationship with wheat. Due to its high nutritional value, and the absence of gluten, this flour is ideal for the preparation of celiac products, and its use as an ingredient of foods considered “ecological” is currently increasing.
Several cases of hypersensitivity reactions to buckwheat have been described, mainly in Japan where, due to high local consumption, it causes up to 3% of cases of anaphylaxis in this population.4
The prevalence of respiratory symptoms in an occupational setting among bakers is high: 5%–10% for asthma and 15%–20% for rhinitis.6,7 Sensitization is 4.2% per person per year in exposures of less than 4 years8 (1.0% in longer exposures),9 and this rate increases at higher doses of allergen, especially in atopic patients.6 In bakers, the causative allergens are mostly high molecular weight flour proteins, but other agents present at all stages, from cereal production to bread making (pesticides, contaminants such as mites, fungi, enzymes, etc.), must be taken into account. Buckwheat is a pseudocereal that contains several high molecular weight proteins and, like other allergenic sources, requires a period of exposure to induce sensitization that produces an IgE-mediated hypersensitivity reaction.
Diagnosis requires demonstrating sensitization by skin and/or immunological tests and relating exposure to symptoms. SBCT is the gold standard for diagnosing occupational asthma, as it is the only test that establishes an etiological diagnosis through controlled exposure to increasing doses of the suspected agent while monitoring FEV1.
The most effective preventive method is to control the level of allergenic exposure in order to reduce the number of sensitized workers. Reducing exposure and using protection may reduce symptoms, but the only measure that improves lung function is to avoid exposure.10,11
The importance of this case lies in the scarce availability of literature on occupational asthma due to buckwheat sensitization.12–15 According to hospital records, it can induce serious reactions, although these are rare.3–5 The absence of studies and underdiagnosis due to lack of suspicion make it difficult to estimate the prevalence of this allergy.
Buckwheat is also becoming more prominent in the food sector in Europe because of increased consumption of gluten-free foods. The need for it to be declared as a food allergen should be considered to avoid accidental exposures with significant risks.
In memory of Dr. Eulalia Camino (our beloved Lali).
Please cite this article as: Pascual Erquicia S, Bernaola Abraira M, Dorado Arenas S, Urrutia Landa I, Arrizubieta Basterrechea I, Bronte Moreno O, et al. Rinoconjuntivitis y asma ocupacional por alergia a harina de trigo sarraceno. Arch Bronconeumol. 2020;56:466–468.