We report the case of a 55-year-old woman, former smoker since September 2012 (18 pack-years), with a history of allergic rhinoconjunctivitis and bronchial asthma. No infiltrates were observed in a chest X-ray performed in 2012. Skin prick tests showed sensitization to cat dander and grass and olive pollen.
She was admitted in 2014 for an acute episode of dyspnea, breath sounds, and non-productive cough without fever. Chest X-ray revealed an alveolointersticial pattern predominantly in the lung bases. Chest computed tomography showed bilateral patchy ground glass infiltrates. Bronchoscopy was performed with transbronchial biopsy and bronchoalveolar lavage: neutrophils: 11%; eosinophils: 85.9%; lymphocytes: 0.6%. Biopsy showed a histological pattern of pulmonary eosinophilia suggestive of chronic eosinophilic pneumonia (CEP), with a focal pattern typical of organizing pneumonia. Lung function tests highlighted a restrictive pattern with carbon monoxide diffusion changes: FVC 1830 – 59%; FEV1 1410 – 54% and FEV1/FVC 77%. DLCO 32%; KCO 63%; TLC 61%; and RV 86%. All immunological tests were negative; IgE 493UI/ml. In the 6-min walk test, initial saturation was 97%, distance walked 440m, and final saturation 85%.
CEP was diagnosed, with no known occupational or environmental risks, although a relationship with the administration of anti-inflammatories (celecoxib) could not be ruled out. This drug was discontinued, and treatment began with corticosteroids, resulting in both clinical and radiological worsening.
Given the poor response to treatment with corticosteroids, a surgical biopsy was performed, and the pathology study reported squamous-like interstitial pneumonia with eosinophils, consistent with CEP. The patient was placed on the lung transplantation waiting list. Lung function tests prior to the introduction of omalizumab were: FVC 1430 – 47%; FEV1 1120 – 43%; FEV1/FVC 78%; DLCO 24%; KCO 55%; TLC 44%; RV 81%.
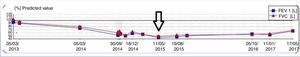
In a review of the literature, 2 cases1,2 of CEP with a favorable response to omalizumab were identified, so treatment began with this drug, producing clinical improvement and functional stabilization, so we decided to gradually withdraw the corticosteroids. Twenty-four months after starting omalizumab, the patient has shown a remarkable improvement in her symptoms without corticosteroids, confirming the reversal of her previous functional decline noted from the introduction of this drug (Fig. 1). The patient was taken off the lung transplantation waiting list when the adverse effects of steroid treatment had resolved. When mepolizumab came on the market, this therapeutic option was proposed to the patient, but she refused it in view of her good progress.
CEP is an idiopathic disease characterized by an abnormal accumulation of eosinophils in the interstitial and alveolar space. Standard treatment is systemic corticosteroids. Response is usually so rapid and favorable, that if no response is observed, alternative diagnoses must be considered.
Our patient presented a poor response to high-dose corticosteroids, so a surgical biopsy was performed, which confirmed the initial diagnosis. We identified 2 cases of CEP with response to omalizumab in the literature1,2 involving patients with elevated IgE and poor response to corticosteroids (or a requirement for high doses). In both cases, treatment with omalizumab reversed deterioration, and produced improvements in lung function tests.
Omalizumab is a humanized anti-IgE antibody, usually indicated for the treatment of persistent allergic asthma. Numerous effects that go far beyond IgE immunomodulation have also been described.3–11 Omalizumab reduces basophil Fc epsilon RI alfa receptor expression.3–5 It also induces a decrease in triptase, Th2 cytokines (IL-4 and IL-13), and chemokines (IL-8 and RANTES), irrespective of IgE levels. Similarly, it reduces cytokine expression (IL-5, IL-10, and IL-13) in dendritic cells,6,7 and interferes with their ability to activate CD4. It also reduces eosinophil numbers8,9 in both sputum and lung tissue, monocytes,9 fraction of expired nitric oxide (FENO),9,10 and endothelin-1 concentrations in exhaled breath condensate.10 Moreover, stimulation of IgE increases the deposit of collagen I, III, and IV, and fibronectin by the Erk1/2 MAPK pathway, thereby increasing airway remodeling. By blocking this action, muscle proliferation and the deposit of pro-inflammatory substances can be reduced.11
Our patient's progress not only demonstrates the favorable effect of omalizumab, but also suggests that it is more than just an IgE immunomodulator, and that its effects on eosinophilic inflammation are also important. These findings are supported by the results of basic research, and have been confirmed by reports of favorable responses, such as in our patient, in other conditions such as Churg-Strauss disease or chronic rhinosinusitis, in which eosinophilic inflammation is a key component.12
Please cite this article as: Laviña-Soriano E, Ampuero-López A, Izquierdo-Alonso JL. Respuesta a omalizumab en paciente con neumonía eosinófila crónica y mala respuesta al tratamiento con corticoides. Arch Bronconeumol. 2018;54:393–394.