Respiratory muscle dysfunction, particularly of the diaphragm, may play a key role in the pathophysiological mechanisms that lead to difficulty in weaning patients from mechanical ventilation. The limited mobility of critically ill patients, and of the diaphragm in particular when prolonged mechanical ventilation support is required, promotes the early onset of respiratory muscle dysfunction, but this can also be caused or exacerbated by other factors that are common in these patients, such as sepsis, malnutrition, advanced age, duration and type of ventilation, and use of certain medications, such as steroids and neuromuscular blocking agents. In this review we will study in depth this multicausal origin, in which a common mechanism is altered protein metabolism, according to the findings reported in various models. The understanding of this multicausality produced by the same pathophysiological mechanism could facilitate the management and monitoring of patients undergoing mechanical ventilation.
Es probable que la disfunción de los músculos respiratorios, principalmente del diafragma, constituya una pieza clave dentro de los mecanismos fisiopatológicos que conducen a la dificultad del destete de la ventilación mecánica. La limitada movilidad del paciente crítico—y en especial del diafragma—cuando se requiere soporte prolongado con ventilación mecánica favorece el inicio temprano de la disfunción muscular respiratoria, la cual puede originarse también o hacerse mayor en presencia de factores frecuentes en el paciente críticamente enfermo, tales como sepsis, desnutrición, edad avanzada, duración y modo ventilatorio, uso de algunos medicamentos como glucocorticoides y bloqueadores neuromusculares. En esta revisión haremos énfasis en este origen multicausal, en el que la alteración del metabolismo de las proteínas es un mecanismo común involucrado, de acuerdo con los hallazgos reportados en diferentes modelos. El entendimiento de esta multicausalidad integrada por un mismo mecanismo fisiopatológico podría favorecer el manejo y la monitorización de los pacientes sometidos a ventilación mecánica.
Mechanical ventilation (MV) is one of the most common means of life support in intensive care units (ICU) and forms part of the standard treatment of acute respiratory failure. However, despite its advantages, MV can cause direct systemic and pulmonary complications1 leading to longer hospital stays, increased costs, higher mortality and loss of quality of life.2 As such, it is essential that the duration of MV in a critically ill patient is kept as short as possible by judicious daily evaluation on the part of the clinician. It has been calculated that around 40% of the total time on MV in the ICU is dedicated to weaning respiratory support.3 Some descriptive studies have shown that 69% of patients are easily weaned, while 15% require prolonged MV (PMV), with hospital stays of over 10 days.4
Difficulty in weaning from MV is a significant problem, since it increases complications like nosocomial infections and/or airways lesions and others. In addition to producing significant deterioration in quality of life, difficulty in weaning consumes up to 40% of all ICU resources.2,5 Respiratory muscle dysfunction, particularly of the diaphragm, may play a key role in the pathophysiological mechanisms that lead to difficulty in weaning patients from MV.6 The limited mobility of the diaphragm under MV promotes the early onset of respiratory muscle dysfunction,2,3 and this can be exacerbated by other factors, such as advanced age, long duration of MV, controlled ventilatory mode, malnutrition, sepsis and some medications, such as glucocorticoids and neuromuscular blocking agents (NMBA).7 Awareness of the pathophysiological mechanisms underlying these factors in respiratory muscle dysfunction8 and their role in difficult weaning is on the increase.
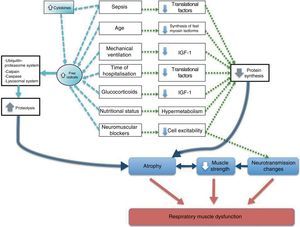
Two aspects are highlighted in this report. The first is that the factors primarily associated with respiratory muscle dysfunction occur frequently and often simultaneously in patients on MV. The second is that the common mechanism underlying the physiopathology of these factors is proteolysis and/or reduced muscle protein synthesis, which has also been shown on histology as atrophy.9
Factors Associated With Respiratory Muscle DysfunctionAgeIn two prospective multicentre studies in mechanically ventilated patients in intensive care units in more than 20 countries in America and Europe10 and in Latin America,11 the average age of patients was 57 years, while that of patients on PMV was 72 years. Generally in humans, skeletal muscle strength, mass and structure change with age. At the age of 70 years, subjects have a reduction of muscle mass of between 20% and 30%, causing a loss of peripheral strength of between 20% and 40%.12 This diminished peripheral mass is the result of a fall in number and size of muscle fibres, principally the fast twitch type.13 Age-related changes may be different in the respiratory muscles and in the peripheral muscles, since respiratory activity is continuous, while peripheral muscle activity may not be. Although data in humans are limited, age-related respiratory muscle dysfunction has been demonstrated by a loss of strength, determined in subjects aged between 65 and 85 years as a yearly reduction in maximum inspiratory pressure (MIP) of 0.8–2.7cmH2O14 and a 25% fall in transdiaphragmatic pressure in adults between 65 and 75 years of age.15 A mechanism that may explain these changes is the accumulative effect of oxygen-derived free radicals that may trigger proteolytic processes.16 It has also been suggested that with advancing age, remodelling occurs in the muscle fibres, with fast twitch myosin fibres being replaced by slow twitch isoforms.12
Duration and Mode of Mechanical VentilationIn reports on the progress of patients admitted to the ICU, 30% needed a mean duration of 5–8 days MV support and the most frequently used mode was assist-control (60%).10,11 Among MV patients, 30% had difficulty weaning and a significant proportion of these became what was defined as PMV. It seems that, in addition to MV duration, ventilatory mode is a determining factor for the development of diaphragmatic muscle dysfunction.17 This was first described in 1994 by Le Bourdelles et al.,18 who submitted rats to MV and showed that maximum muscle strength per unit cross-sectional area fell after 48hours of support. Interest in diaphragm muscle wastage has been growing in recent years.9 Several studies performed in different animal species have shown that significant atrophy of the slow and fast twitch fibres of this muscle occurs after only 12–18hours (h) on MV.17 This occurs before the appearance of atrophy in the musculoskeletal system that has often been described in experimental animal models after 96h of MV.9 Similar results were confirmed in humans after 18–69h of MV9: diaphragm atrophy was seen when biopsies from brain death patients (after undergoing controlled MV) were compared with controls undergoing chest surgery. One important finding was the reduction of the cross-sectional area in both type I and type II fibres in patients receiving ventilation for more than 48h. Some animal studies show that immobility from controlled MV also causes a loss of fibres from the locomotor skeletal muscles, a myofibrillar disorder of the diaphragm, and, furthermore, changes in the Z-line structure in both.19
The mechanism mainly associated with diaphragm atrophy in animal models20 and in humans undergoing MV is the increase in proteolysis.9,21 In animals, a reduction in protein synthesis has also been observed.18,20 The contribution of calpain, caspase-3, and the lyosomal and the ubiquitin-proteasome systems has been discussed in recent studies.8 Current research is directed towards the transduction pathways of these mechanisms, with the aim of identifying drugs or therapeutic interventions that would deviate these pathways towards the prevention of atrophy and respiratory muscle dysfunction. In this respect, alternatives, such as reducing the time of controlled mode MV, transcutaneous electric stimulation of the diaphragm, early mobilisation of patients22 and the use of antioxidant drugs, have been proposed.
Nutritional and Metabolic StatusBetween 30% and 60% of ICU patients have or will have some degree of malnutrition, due to metabolic changes causing a greater energy output and the nutritional deficit due to poor absorption or reduced availability of nutrients during critical disease.23 The increase in catabolic hormones (glucagon, adrenaline and cortisol) and cytokines24 and the inhibition of anabolic hormones, such as insulin and testosterone, produces a situation of hypermetabolism. A hypermetabolic patient will suffer a loss of muscle mass and strength and immune response.24 Hormone imbalance has frequently been associated with the development of hyperglycaemia. Although this is a condition that adapts to critical disease, it remains a factor for negative prognosis in the short, mid and long-term.25 Hyperglycaemia aids the storage of lipids in the form of triglycerides and low density lipoproteins.26 The unavailability of these substrates as energy sources leads to marked proteolysis, and as such, to a loss of muscle mass, an increase in severe infections, multiple organ failure and death, particularly in critically ill surgical patients.27 The weight of the diaphragm in a malnourished rat drops more than the weight of the muscles of the limbs, as a result of atrophy and remodelling of fast twitch fibres.28 In addition, hyperglycaemia causes oxidative stress, which has been associated with nerve fibre loss and atrophy, with the corresponding impact on muscular neurotransmission.
ComorbiditiesCritically ill patients undergoing MV may present various comorbidities, the most common being sepsis, diabetes mellitus, hypertension and acute myocardial infarction. Complications such as barotrauma, sepsis, acute respiratory distress syndrome (ARDS), MV-related pneumonia, cardiogenic shock and polyneuropathy in critically ill patients may also occur.10 The effects of these diseases in the development of respiratory muscle dysfunction due to mechanisms mediated by changes in protein metabolism may be additive. For example, in both animals and humans, the systemic inflammatory response in sepsis induces an increase in proinflammatory cytokines (TNF-α, IL-6, IL-1) and free radicals,29 which also promote greater activity of the proteolytic pathways,30 as mentioned above. With regard to protein synthesis in the skeletal muscle of rats, it has been reported that other sepsis-induced inflammatory mediators, such as IL-1β, reduce eIF4G factor phosphorylation, thus altering the onset of translation of sarcoplasmic proteins, such as myofibrils, in muscles composed of fast twitch fibres.31 Mechanisms other than changes in protein metabolism regulation have been proposed in sepsis; mechanisms that are associated with changes in cell excitability, calcium homeostasis30 and mitochondrial oxidative phosphorylation of the muscle.
Pharmacological TreatmentGlucocorticoidsGlucocorticoids (GC) are used in the critically ill patient with sepsis, acute respiratory distress syndrome (ARDS) and refractory vasodilatory shock.32 High doses have been associated with neuromuscular disorders causing peripheral and respiratory muscle dysfunction. In patients on MV, GC have been seen to delay MV weaning and to increase the need for tracheostomy.32
In humans and animals, GC-induced respiratory and peripheral muscle dysfunction is caused by inhibition of anabolism and by the catabolic effect of proteins.33 The anti-anabolic effect of the GCs inhibits protein synthesis by various mechanisms. One of these is the inhibition of amino acid transport within the muscles, limiting protein synthesis. Another mechanism that has been proposed is the inhibition of the stimulating effect of insulin and the insulin growth factor (IGF-1) on the phosphorylation of the eIF4-binding protein and ribosomal protein kinase S6, two key factors in mRNA translation.33 Finally, GCs inhibit myogenesis by the low regulation of myogenin, an essential transcription factor for the differentiation of satellite cells in muscle fibres.34 Stimulation of IGF-1 or the myostatin blockers constitute some of the more promising therapeutic targets for preventing GC-induced muscle atrophy. The catabolic action of GCs is mediated by the proteolytic ubiquitin-proteasome, lysosome and calpain-dependent systems35 that primarily affect the myofibrillar proteins. In muscle wasting, intracellular mediators such as FOXO, GSK3b, C/EBPb, p300, REDD1 and ATF4 form part not only of the catabolic action but also of the inhibitory action of GC anabolism.35
Neuromuscular Blocking AgentsNMBAs are used to improve synchrony in MV patients and to keep the ventilatory parameters high (PEEP>10cmH2O, FIO2>80%), when required. NMBAs are either depolarising or non-depolarising. In a study on rat diaphragm comparing the effects of these agents, non-depolarising NMBAs were found to be more potent.36 In humans, it has been reported that NMBAs did not cause ICU-acquired weakness compared to placebo.37 However, respiratory complications (prolonged desaturation, SatO2<90%) requiring re-intubation were reported in some publications.38
Prolonged use of high-dose NMBAs together with steroids in the presence of prolonged immobilisation promotes muscle weakness in the critically ill patient and, in some cases, acute necrotising myopathy.39 This condition progresses with generalised weakness of the peripheral and respiratory muscles, recovery is slow and patients are left with sequelae. In critically ill patients with sepsis or multiple organ failure, NMBA pharmacokinetics are altered due to changes in physical function, perfusion and the intracellular/extracellular fluid ratio.40 In the light of these findings, intermittent dosing with NMBAs that do not change kidney or liver function is recommended.
Respiratory Muscular Dysfunction Synthesis in the Critically Ill Patient Undergoing Mechanical VentilationIn the schematic in Fig. 1, the factors contributing to respiratory muscle dysfunction in the critically ill patient on MV are presented. The mechanisms involved in protein breakdown and/or the reduction of protein synthesis for each factor are listed.
ConclusionAlthough respiratory muscle dysfunction in the critically ill patient undergoing MV has multicausal origins, the primary underlying mechanisms may be proteolysis and/or the reduction of protein synthesis, and in some cases, neurotransmission disturbances. Respiratory muscle dysfunction causes difficulty in weaning, PMV, and morbidity and mortality in the critically ill patient.
Although the aim of this review was to focus on respiratory muscle dysfunction, the peripheral musculature is also affected in one way or another by the multicausal nature of this disorder and its associated mechanisms.
RecommendationsEarly, integrated management of the multiple causes of respiratory muscle dysfunction may reduce hospital stay and associated morbidity and mortality, and could prevent the development and severity of the sometimes irreversible neuromuscular sequelae.
It is important that research into the quantification and regulation of altered protein metabolism in these patients continues, with the aim of counteracting this metabolic tendency with a series of treatment prescriptions and diets more closely suited to the real conditions of the patient undergoing MV.
FundingCall for Grants, Universidad del Valle, 2010.
Framework AgreementFundación Valle del Lili and Universidad del Valle.
Conflict of InterestsThere is no institutional or individual conflict of interests.
This study was made possible thanks to the institutional support provided by Universidad del Valle and Fundación Valle del Lili (FVL), Cali-Colombia. We would also like to thank Dr. Mónica P. Vargas, MD, Anaesthesiologist, Intensive Care Unit, FVL.
Please cite this article as: Díaz MC, Ospina-Tascón GA, Salazar C BC. Disfunción muscular respiratoria: una entidad multicausal en el paciente críticamente enfermo sometido a ventilación mecánica. Arch Bronconeumol. 2014;50:73–77.