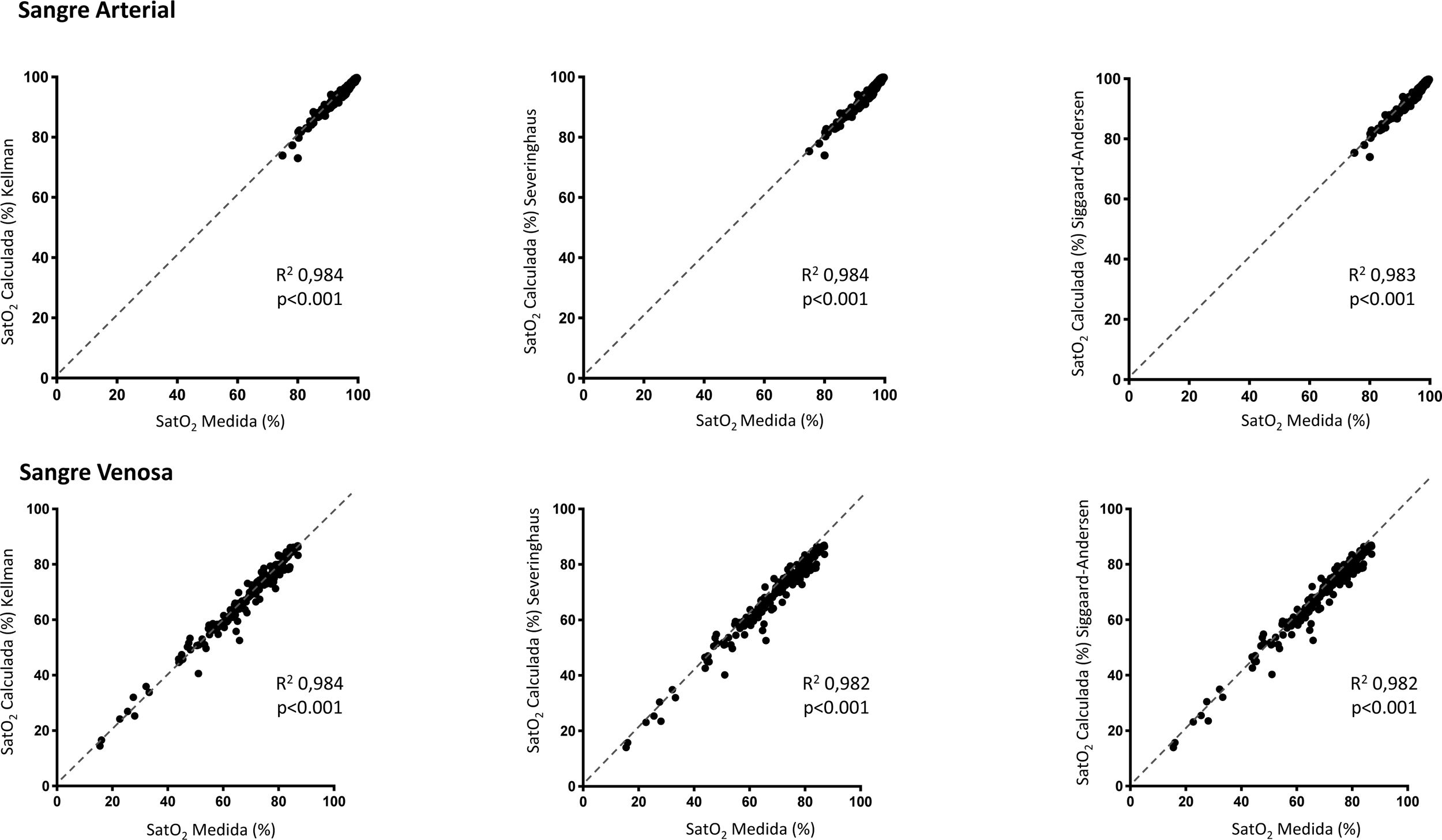
We read with interest the scientific letter from Prof. Böning et al.1 commenting on our article on the affinity of hemoglobin for oxygen in patients with COVID-19.2 The aim of our study was to reply from a clinical point of view to the hypothesis generated by two basic research papers that suggested that the virus decreases this affinity by way of different mechanisms.3,4 We, like previous authors such as Gille et al.5 and Laredo et al.,6 found that the virus appears to have little effect on the interaction of hemoglobin with oxygen. However, these results contrast with those published by other authors, such as Vogel et al.7 It is important for the management of patients that these discrepancies are clarified, since the clinical impact of this affinity affects the real value of PaO2 as an indicator of blood oxygenation. The dispersion of our data, which included hospitalized patients with COVID-19 of heterogeneous severity, prompted Prof. Böning's group of physiologists to suggest that a reduced affinity between hemoglobin and oxygen may be a particular problem in more serious patients. They also suggest that this may be caused by shifts in the oxygen–hemoglobin dissociation curve, due, for example, to changes in the concentration of 2–3 diphosphoglycerate (2.3-BPG). Unfortunately, we did not determine blood levels of this 1.3-diphosphoglycerate isomer, which, together with several other variables that were analyzed in our study (PaCO2, pH, temperature), affects the shape of the above-mentioned curve. We reanalyzed our data, including only the group of patients admitted to the intensive care unit for lung involvement that led to respiratory failure (n=75, with a total of 343 arterial and 220 venous samples), but this procedure did not reveal any relevant discrepancies between measured and calculated saturation (Fig. 1), so we conclude that there does not appear to be a loss of normal affinity of hemoglobin for oxygen. The possible decrease in hemoglobin itself, another parameter that varies considerably among clinical studies,7,8 could be due to different causes, such as the viral disease itself, nutritional deficiencies, or the proinflammatory state of critical patients. Another cause could be the frequent repetition of laboratory tests in intensive care units,9 a practice that was particularly common for both healthcare and for research reasons in severe COVID-19 patients. However, the rate of anemia in our severe patients was 27.8% (mean hemoglobin 12.1±1.9g/dl), even lower than in critical patients with other diseases.10 It should be noted here that our hospital was very restrictive with regard to blood draws for research: a single sample was drawn from each patient and competitively allocated among the various studies.
Conflict of interestsThe authors state that they have no conflict of interests.