Ganglioneuromas are benign neurogenic tumors that can invade or adhere strongly to the mediastinal structures, producing varying clinical manifestations.1 We present a case of brachial neuralgia due to compression of the brachial plexus by a mediastinal ganglioneuroma.
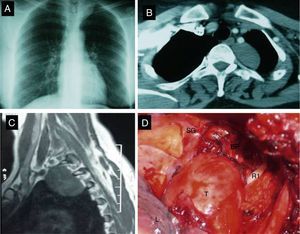
A previously healthy 39-year-old woman was hospitalized for a 3-month history of brachial neuralgia (BN) in the left arm. Physical examination was normal. Left laterotracheal opacity was detected on chest X-ray (Fig. 1A). A well-defined tumor in the left paravertebral region, 6cm in diameter, with some areas of intravenous contrast medium uptake was found on chest computed tomography (CT) (Fig. 1B) and magnetic resonance imaging (MRI) (Fig. 1C). The mass was not compressing the spinal cord and there was no direct invasion of the vertebrae. Laboratory test results and bronchoscopy were completely normal. The apical mass and part of the sympathetic chain were extracted via a left posterolateral thoracotomy (Fig. 1D). The mass showed strong adhesions to the brachial plexus and the stellate ganglion, with widening of the intervertebral space. The pathology report confirmed the diagnosis of ganglioneuroma, in view of the mature ganglion cells contained in a stroma of collagen fibers with the presence of some Schwann cells. In the post-surgical period, the patient presented transient Claude Bernard–Horner syndrome that resolved fully after 2 months. Clinical examination and CT at 3 and 6 months of follow-up were favorable.
(A) Chest X-ray showing left paratracheal opacity. (B) Chest computed tomography showing an encapsulated mass in the left posterosuperior mediastinum at the T2–T3 level. (C) Chest magnetic resonance image: well-defined tumor in the left paravertebral region with no compression of the spinal cord and no direct vertebral invasion. (D) Direct image of ganglioneuroma during surgery. R1: first rib; SG: stellate ganglion; L: lung; BP: brachial plexus; T: tumor.
Ganglioneuroma, originating in the neural crest cells, is the most mature form of neuroblastoma. It occurs most frequently in the mediastinum (70%)2,3 and age at presentation is generally young.4 Most cases are asymptomatic. In the series of Takeda, 67% of cases were asymptomatic, while only 1.4% had neurological symptoms and 2 cases of paresthesia of the arm. Some symptoms are related with the secretion of hormones, such as vasoactive intestinal peptide, causing diarrhea, or catecholamines that produce adrenergic symptoms (hypertension, palpitations or sweating), but our patient did not present any symptoms of this kind.5
On CT and MRI, ganglioneuroma is seen as a solid, well defined, encapsulated mass. Around 10% of neurogenic paravertebral tumors have an extension into the vertebral canal and thus are called ‘dumbbell tumors’, as was the case in our patient.
Spinal cord invasion by the tumor can be more precisely determined on MRI, so this evaluation must be performed before surgery in patients with suspected neurogenic tumor in order to rule out any intramedullary extension. Surgical resection is the standard treatment. The transmanubrial approach provides an excellent surgical field, with control of the subclavian vessels, the brachial plexus and exposure of the upper cervical and dorsal spine. Cardillo et al.1 concluded that video-assisted surgery (VATS) was associated with lower morbidity and a shorter post-surgery hospital stay. The possibility of using VATS depends on tumor size and intramedullary extension. In our case, we decided to perform a thoracotomy, since surgery of the thoracic apex carries a greater risk of vascular or nervous injury, and also because greater control of the intraspinal extension of the tumor was required. Our case is unusual, in that the ganglioneuroma was exceptionally large and the first symptom leading to diagnosis was brachial neuralgia.
Neurological symptoms such as cervical and brachial neuralgia may be a sign of mediastinal tumor.
Conflict of InterestsThe authors declare that they have no conflict of interests.
Please cite this article as: El Hammoumi M, Arsalane A, Kabiri EH. Ganglioneuroma mediastínico posterior. Arch Bronconeumol. 2015;51:50–51.