Chylothorax is the accumulation of chyle in the pleural cavity caused by damage to the thoracic duct or any of its branches.1 It contains a high concentration of triglycerides in the form of chylomicrons, giving chyle its milky appearance.1 The definitive diagnosis is based on the characteristic finding of chylomicrons or triglyceride levels greater than 110mg/dl.1 It is divided into 2 groups: traumatic (both iatrogenic and non-iatrogenic), and non-traumatic (malignant, miscellaneous or idiopathic).1 In the case of non-traumatic chylothorax, treatment of the underlying disease is indicated, and unless the etiology is malignant, a long-chain triglyceride-free diet is recommended.2 In traumatic chylothorax, initial treatment should be conservative, although early surgery is recommended if the volume is very large.1
We report the case of a patient who presented recurrent right chylothorax due to vena cava obstruction, caused by occlusion of a subcutaneous venous reservoir inserted for previous chemotherapy (CT). The patient was treated surgically by opening the right vena cava, resecting the fibrosis, and using a heterologous bovine pericardium patch for repair, with a good outcome.
This was a 57-year-old woman diagnosed in 2014 with squamous cell carcinoma of the anal canal (T4N2), treated initially with CT and neoadjuvant radiation therapy (RT), followed by surgery. She was referred by the oncology clinic to the emergency department with a 1-month history of dyspnea on moderate exertion, accompanied in recent days by right pleuritic chest pain. Lung auscultation revealed reduced breath sounds in the right hemithorax, while the rest of the examination was normal. Chest X-ray on admission showed moderate-large right pleural effusion. Thoracentesis yielded a milky fluid, typical of chylothorax, and cytology was consistent with inflammation.
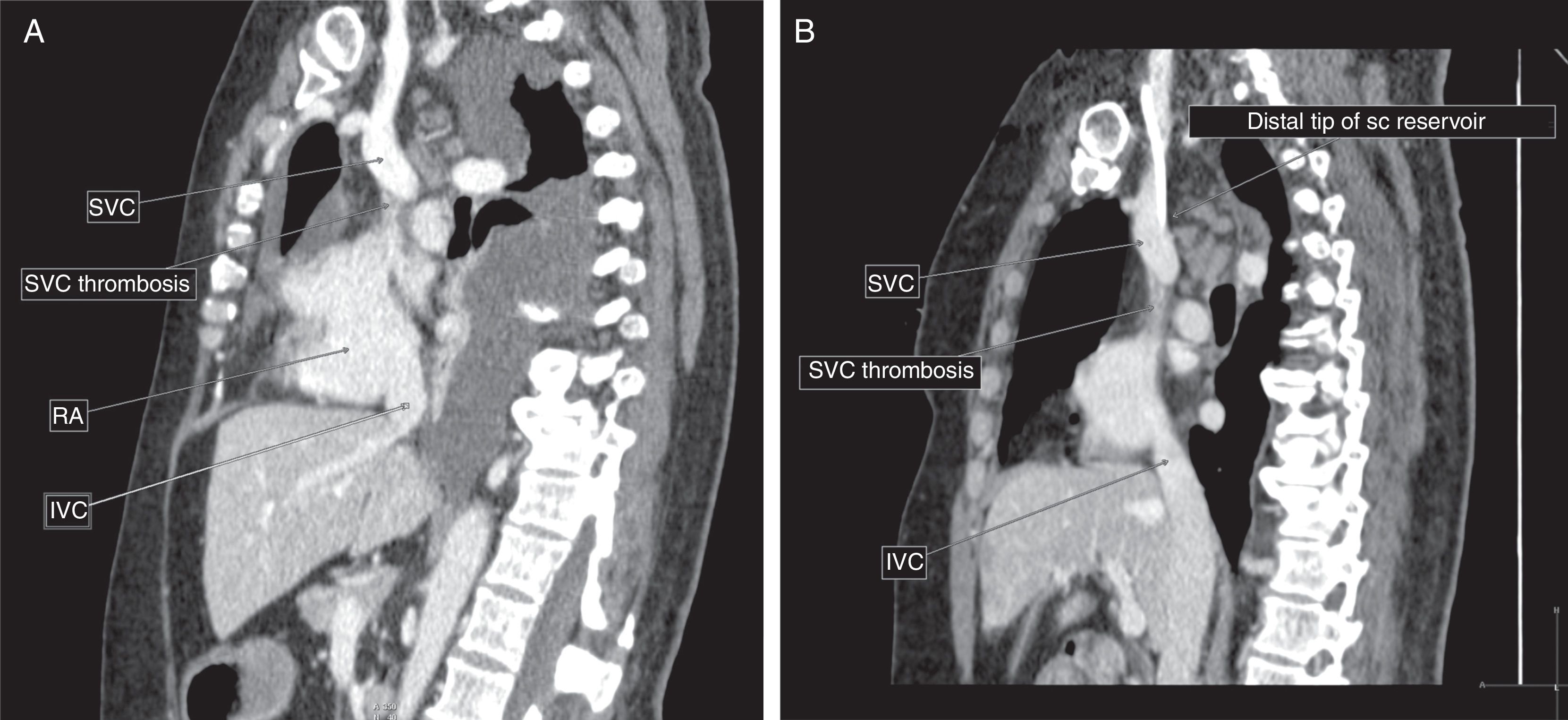
In view of the findings, a chest tube was placed and the patient began a specific protein-rich, low-fat diet, with supplements of medium-chain triglycerides and exclusion of long-chain triglycerides. Chest computed tomography (CT) (Fig. 1) showed thrombosis of the superior vena cava from the mouth of the azygos vein to its entry into the right atrium, so the implanted vascular reservoir was removed. The patient was also evaluated by the hemostasis and peripheral vascular surgery units, and anticoagulation for at least 3 months was recommended, initially with low molecular weight heparin and later with acenocumarol. The patient progressed well during admission and was discharged with anticoagulant treatment and specific dietary recommendations for chylothorax. Initial clinical and radiological progress was good, so a normal diet was reinstated.
(A) Computed tomography with intravenous contrast in the venous phase. Sagittal slice. A superior vena cava filling defect is visualized proximal to the mouth of the arch of the azygos vein, extending to the entry into right atrium, consistent with at least partial thrombosis of the structure, and associated with significant effusion. (B) Sagittal slice. Distal tip of the subcutaneous reservoir in relation to the subcutaneous vena cava thrombosis. IVC: inferior vena cava; RA: right atrium; sc: subcutaneous; SVC: superior vena cava.
In a routine check-up 4 months after discharge, the patient reported a 2-week history of worsening dyspnea. Chest X-ray showed the reappearance of pleural effusion. Chest CT revealed a significant amount of right pleural effusion with atelectasis of the underlying parenchyma and persistent narrowing of the superior vena cava from the mouth of the azygos vein to its entry in the right atrium, probably at least partially thrombosed, with no significant changes since the last study. The patient was admitted, a new chest tube was placed, and the low-fat diet was reinitiated. In view of the recurrent chylothorax with persistent superior vena cava thrombosis, evaluation by the cardiac surgery department was requested. After assessing the case, surgery was performed, with median sternotomy and cannulation of the right jugular and femoral veins and aortic artery. The superior vena cava was opened longitudinally, and found to be completely occluded by fibrosis. The fibrosis was resected and repair was performed with a heterologous bovine pericardium patch. The pathology study reported fibroconnective tissue with no evidence of neoplastic infiltration or thrombotic material.
Post-surgical progress was favorable, so the patient was discharged with a prescription for acetylsalicylic acid (100mg/day) and specific diet. Her clinical progress remained favorable in subsequent check-ups, and complete radiological resolution of pleural effusion was confirmed.
Neoplasms (lymphoma, chronic lymphocytic leukemia, and metastatic cancer) are the main causes of non-traumatic chylothorax,1 and after prolonged assessment of the patient many cases of chylothorax initially thought to be idiopathic are later found to be associated with occult neoplasms. The less common causes of non-traumatic chylothorax include sarcoidosis, tuberculosis, lymphangioleiomyomatosis, venous thrombosis, superior vena cava syndrome, chest irradiation, thoracic duct thrombosis, and constrictive pericarditis.1 In venous thrombosis, chylothorax is caused by venous obstruction that hinders thoracic duct drainage. It can occur due to medical conditions or non-surgical trauma, such as central venous catheter placement.3
Long-term central venous catheters can cause superior vena cava syndrome, especially when the tip of the catheter is located above the cavoatrial junction. Image-guided catheter placement helps prevent superior vena cava obstruction.4 The use of permanent venous catheters and cardiac pacemakers has increased in recent decades, prompting an increase in the incidence of superior vena cava thrombosis.4
Superior vena cava syndrome due to benign disease requires prompt and durable treatment because affected patients frequently have long life expectancies.5 First-line treatment is conservative management with anticoagulation, but refractory symptoms may warrant intervention.5 The 2 main invasive treatments are percutaneous endovascular repair and open surgical reconstruction. Both have demonstrated efficacy over the mid-term, but surgical reconstruction is the only method with proved patency over the long term.5
Please cite this article as: Cerezo Lajas A, Martín Pinacho JJ, Frías Benzant I, de Miguel-Díez J. Quilotórax recidivante por obstrucción de la vena cava secundaria superior. Arch Bronconeumol. 2018;54:434–435.