Hepatic radioembolization is a recognized technique that uses yttrium-90 (I-90) in the treatment of hepatocellular carcinoma (HCC) and liver metastases.1 On rare occasions (less than 1% of cases), this treatment causes radiation pneumonitis.2,3 We report a case of lung toxicity probably caused by I-90 hepatic radioembolization and explain the underlying pathophysiology.
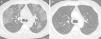
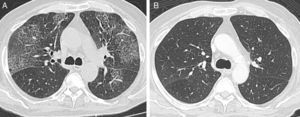
A 73-year-old man, former smoker with a history of alcoholic cirrhosis and unresectable HCC, consulted due to a 1-month history of progressive dyspnea on exertion. Two months before the consultation, he had undergone hepatic radioembolization with I-90 resin microspheres, with an expected lung dose of 10Gy. Before treatment, lung scintigraphy after injection of technetium-99m-labeled albumin macroaggregates (MAA-99mTc) in the hepatic artery had revealed a lung shunt fraction of 10%. On physical examination, the patient presented tachypnea, bilateral crackles on pulmonary auscultation, and peripheral oxygen saturation of 88%, with no signs of heart failure. Chest computed tomography revealed a “crazy paving” pattern, with elevation of the right hemidiaphragm (Fig. 1A). The need for a diagnostic bronchoscopy was discussed, but refused by the patient. Given his history of radioembolization and hepatopulmonary shunt, a presumptive diagnosis of pneumonitis due to radioembolization was established. Treatment began with 20 mg/day prednisone for 2 months, and the patient's clinical condition improved with resolution of changes on tomography (Fig. 1B).
Radiation pneumonitis following hepatic radioembolization with I-90 microspheres has previously been reported. The pathophysiology of this phenomenon involves a shunt between the hepatic arterial circulation and the pulmonary circulation. This shunt is associated with certain liver tumors that lead to the development of abnormal vascular communications. The probability of this complication occurring is proportionate to the magnitude of the hepatopulmonary shunt,2 so this ratio must be calculated during the treatment planning angiogram by administering a radioactive tracer (MAA-99mTc) to the hepatic artery and performing a quantitative lung scintigraphy. The shunt fraction is calculated as the ratio between the dose administered and the dose recorded on the lung scintigraphy. If ≥20% or a lung exposure of >30Gy in a single dose or 50Gy in accumulated does is predicted, radioembolization is contraindicated.4,5
Clinical symptoms include cough, dyspnea and fever. Tomography findings appear 1–2 months after therapy in the form of ground glass infiltrates and septal thickening. The treatment of choice is systemic corticosteroids.2 Our patient presented clinical and radiological findings consistent with radiation pneumonitis. It is important that this complication is recognized, and it must be taken into account among patients undergoing hepatic radioembolization.
Please cite this article as: Castro HM, Wainstein EJ, Maritano Furcada J. Neumonitis por radiación secundaria a radioembolización hepática con itrio-90. Arch Bronconeumol. 2017;53:216–217.