A holistic approach, including psychological support, participation to rehabilitation programs and nutrition management, has been proposed for chronic pulmonary diseases including idiopathic pulmonary fibrosis (IPF).1,2
Prevalence of depression and anxiety ranges between 14 and 60% in patients with pulmonary fibrosis and both of them are associated with worse outcomes, although are often overlooked and undertreated.1,3
Rehabilitative interventions are recommended by international guidelines,4 but the few data available from national registries show that only less than 20% of the patients are referred to rehabilitation programs.5–7
Signs of nutritional and physical performance impairment, including unintentional weight loss and low hand grip strength, have been observed early in the disease course with a further worsening already after 6-month of follow-up.8,9 Furthermore, malnutrition has been associated with worse clinical outcomes.10
Despite the increasing evidence, recent IPF guidelines do not provide specific recommendations for referral to the above mentioned specialists.
Real-life data on the inclusion of patients in rehabilitation programs and referral to psychological and nutritional counseling are lacking. Furthermore, there are no data regarding the implementation in clinical practice of specific questionnaires to help pulmonologists to identify IPF patients who may benefit from a holistic approach.
The aim of this study is to evaluate the proportion of patients with IPF who are referred to these specific interventions and the role of questionnaires in supporting the decision-making process.
Sixty-nine consecutive patients (median [IQR] age: 76 [71–79] years; 20 [29.0%] females) followed-up at the IPF clinic of the IRCCS “San Gerardo dei Tintori” Monza, Italy between October 2022 and March 2023 were enrolled in the study. The patients underwent a pneumological visit during which the following data were collected: respiratory symptoms, physical exam, pulmonary function tests, 6-minute walking test (6MWT) and body mass index (BMI). The majority of patients were in Gender, Age and Physiology (GAP) stage I and II (28 [40.6%] and 33 [47.8%], respectively), while only 8 (11.6%) patients were in GAP stage III. The study received Ethics Committee approval.
At every visit, two IPF expert pulmonologists (AB and FL) answered the following 3 questions based on their clinical judgment: (1) “Does this patient require psychological support?”; (2) “Does this patient require nutritional intervention?” and (3) “Should this patient be referred for pulmonary rehabilitation (PR)?”. The only two possible answers to the prior questions were “yes” or “no” and the two pulmonologists were asked to reach a consensus between them, without other supporting tools.
Before the visit, the patients were asked to fill out 3 self-administered questionnaires: (1) International Physical Activity Questionnaire (IPAQ); (2) Mini Nutritional Assessment (MNA), and (3) Hospital Anxiety and Depression Scale (HADS).11–13 These questionnaires were collected by nursing personnel, while the two IPF experts remained blinded.
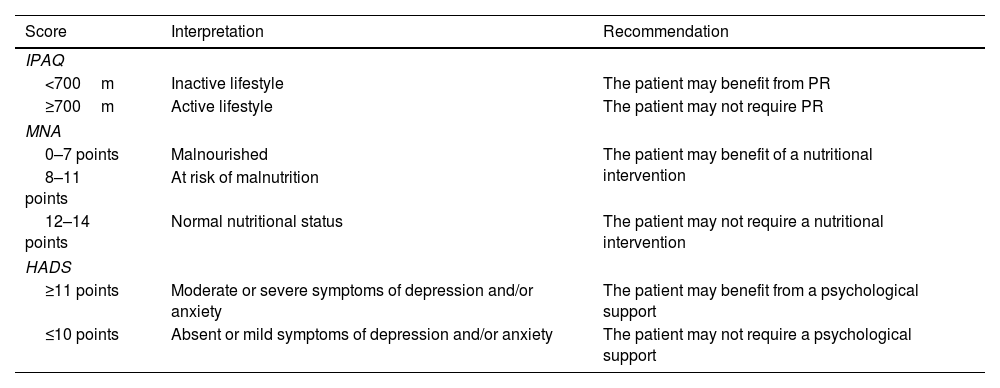
The results of the questionnaires were interpreted as summarized in Table 1.
Interpretation of the Questionnaires.
| Score | Interpretation | Recommendation |
|---|---|---|
| IPAQ | ||
| <700m | Inactive lifestyle | The patient may benefit from PR |
| ≥700m | Active lifestyle | The patient may not require PR |
| MNA | ||
| 0–7 points | Malnourished | The patient may benefit of a nutritional intervention |
| 8–11 points | At risk of malnutrition | |
| 12–14 points | Normal nutritional status | The patient may not require a nutritional intervention |
| HADS | ||
| ≥11 points | Moderate or severe symptoms of depression and/or anxiety | The patient may benefit from a psychological support |
| ≤10 points | Absent or mild symptoms of depression and/or anxiety | The patient may not require a psychological support |
IPAQ=International Physical Activity Questionnaire; MNA=mini nutritional assessment; HADS=hospital anxiety and depression scale.
Categorical variables were reported with absolute and relative frequencies, continuous variables with median and interquartile range (IQR). For each assessment (i.e., nutritional, physical and psychological status), Cohen's Kappa Statistic was used to assess the agreement between the pulmonologists’ clinical judgment and the results of the self-administrated questionnaires.14 Corresponding 95% confidence interval (95% CI) were also reported.
In regards to the psychological support, 54 (78.3%) cases did not require any intervention in the opinion of the IPF experts, while 15 (21.7%) patients required a specialistic support.
According to the HADS results, 57 (82.6%) patients had moderate or severe anxiety and depression scores, while 4 (5.8%) patients had mild or absent anxiety and depression and 8 (11.6%) patients did not complete the questionnaire.
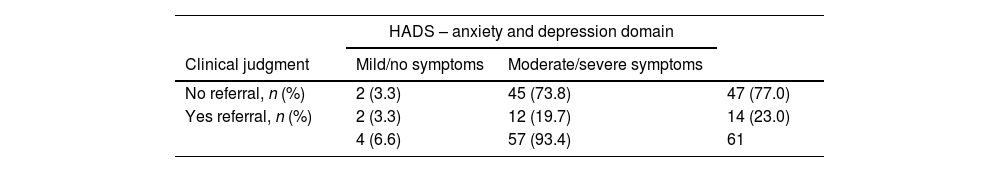
The Cohen's Kappa evaluating the agreement between pulmonologists’ clinical evaluation and the results of the HADS was −0.05 (95% CI: −0.14; 0.05), indicating a very low agreement. Only in 14 out of 61 patients (23.0%) there was agreement between the two methodologies, Table 2.
Agreement Between Clinical Judgment and Questionnaires.
| HADS – anxiety and depression domain | |||
|---|---|---|---|
| Clinical judgment | Mild/no symptoms | Moderate/severe symptoms | |
| No referral, n (%) | 2 (3.3) | 45 (73.8) | 47 (77.0) |
| Yes referral, n (%) | 2 (3.3) | 12 (19.7) | 14 (23.0) |
| 4 (6.6) | 57 (93.4) | 61 | |
| MNA screening score – nutritional domain | |||
|---|---|---|---|
| Normal nutritional status | Risk of or overt malnourishment | ||
| No referral, n (%) | 36 (56.3) | 11 (17.2) | 47 (73.4) |
| Yes referral, n (%) | 3 (4.7) | 14 (21.9) | 17 (26.6) |
| 39 (60.9) | 25 (39.1) | 64 | |
| IPAQ – rehabilitation domain | |||
|---|---|---|---|
| Active lifestyle | Inactive lifestyle | ||
| No referral, n (%) | 28 (59.6) | 16 (34.0) | 44 (93.6) |
| Yes referral, n (%) | 2 (4.3) | 1 (2.1) | 3 (6.4) |
| 30 (63.8) | 17 (36.2) | 47 | |
IPAQ=International Physical Activity Questionnaire; MNA=mini nutritional assessment; HADS=hospital anxiety and depression scale.
In regards to the nutritional management, 51 (73.9%) cases did not require any intervention in the opinion of the IPF experts, while 18 (26.1%) patients required a specialistic support.
According to the MNA screening score, 3 (4.3%) patients were malnourished and 22 (31.9%) at risk of malnutrition, while 39 (56.5%) patients had a normal nutritional status and 5 (7.2%) did not complete the questionnaire.
The Cohen's Kappa for agreement between the pulmonologists’ clinical judgment and the results of the MNA screening score was 0.51 (95% CI: 0.30; 0.73), indicating a moderate agreement. In 50 out of 64 patients (78.1%) there was agreement between the two methodologies, Table 2.
In regards to PR referral, 62 (89.9%) cases did not require any intervention in the opinion of the IPF experts, while 7 (10.1%) patients required specialized support. The severity of the disease (evaluated through GAP stage) did not influence the clinical judgment in regards to this domain.
In contrast, according to the IPAQ results, 10 (14.5%) patients had a sufficiently active lifestyle and 20 (29.0%) had a very active lifestyle, while 17 (24.6%) patients had an inactive lifestyle and 22 (31.9%) did not complete the questionnaire.
The Cohen's Kappa for agreement between pulmonologists’ clinical evaluation and the results of the IPAQ was −0.01 (95% CI: −0.18; 0.16), indicating a very low agreement. Only in 29 out of 47 patients (61.7%) there was agreement between the two methodologies, Table 2.
The results of the MNA and IPAQ did not correlate with the BMI and the meters walked 6MWT, respectively, as shown in Supplementary Tables 1 and Table 2. On one hand, 11 out of 22 patients that were at risk of malnutrition according to MNA were overweight (5 cases), obese (5 cases) and severely obese (1 case). On the other hand, 6 out of 16 patients with an inactive lifestyle according to IPAQ walked equal or more than 350m at 6MWT.
To our knowledge, this is the first study evaluating the role of specific questionnaires in supporting the pulmonologists in the referral of patients with IPF to other specialist services. Our results showed a very low agreement between the clinical judgment and the results of HADS and IPAQ questionnaires in identifying patients that may benefit from psychological and PR support, respectively. In particular, the questionnaires identified a higher number of patients that may benefit from specialist intervention compared to the evaluation of the IPF experts: 45, 11 and 16 patients identified with HADS, MNA and IPAQ, respectively, would not have been identified at clinical judgment only.
Nevertheless, a moderate agreement was observed between clinical judgment and MNA screening score in identifying patients to refer to the nutritionist service.
Furthermore, prior studies conducted in patients both with and without respiratory diseases highlighted the prognostic role of IPAQ, a higher score being associated with better outcomes, such as lower mortality rates and improved pulmonary function tests.15,16
Real life studies performed in different European countries already showed that, despite IPF guidelines recommendations, only a minority of patients are referred to PR programs (<20%), which is in line with our data; in fact only 10% of patients would have been referred to PR programs in the opinion of the IPF experts.1 Using the IPAQ, the proportion of patients who would have required PR increased to 24.6%. Similar results are observed for anxiety and depression, where the number of patients identified with clinical judgment was low (22.0%), while the questionnaires identified a much higher amount of cases (82.6%).
These data support the inclusion of further specialists in the multidisciplinary discussion with the aim to better characterize these specific domains in IPF management.
We also acknowledge some limitations. First of all, the study was conducted in a single center which may limit the generalizability of the results. Secondly, being the questionnaires self-administered, a proportion of patients, particularly for the IPAQ, did not complete the questionnaire leading to missing data. IPAQ is not a multiple choice questionnaire but includes some open questions, and not all patients, particularly elderly, feel comfortable answering this type of questionnaire. This will be the starting point in future studies to use simpler questionnaires, when self-administered, in this group of patients.
In conclusion, the support of specific questionnaires to investigate the nutritional, psychological and physical activity domains may help the pulmonologist, without these expertises, to early identify comorbidities and to refer patients with IPF to psychological support, nutritional evaluation and rehabilitation programs. Questionnaires can give more precise indications than simpler tools already integrated into clinical practice, such as BMI and 6MWT, but they should be easily interpretable by patients. Future studies should evaluate questionnaires designed specifically for patients with IPF on larger cohorts with inclusion of follow-up.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
ContributionsLM and FL are the guarantors of this research. PF, AB and SC were responsible for study concept and design. PF, AB, NA, UZ, VB, MF and FL contributed to patient recruitment and follow-up. PF, AB, NA, UZ, VB, MF and FL contributed to data acquisition. PF, IS, and SC performed data analysis. PF, IS, SC and FB contributed to the drafting of this manuscript. All authors read and approved the final manuscript.
Conflicts of InterestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.
Artificial Intelligence InvolvementArtificial intelligence was not used for the conduct and the writing of this study.
We acknowledge that this research was partially supported by the Grant: Italian MUR Dipartimenti di Eccellenza 2023–2027 (l. 232/2016, art. 1, commi 314–337)