Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is the technique of choice for the study of hilar and mediastinal lymph nodes, useful in the study of lung cancer as well as in benign processes.1 However, diagnosis difficulties have been reported even in benign pathologies.2 Cryobiopsy of lymph nodes (cryoEBUS), a recent and promising technique, improves the diagnostic yield of EBUS-TBNA up to 90%, with a good safety profile.2–4 Few cases of non-malignant disease as sarcoidosis or tuberculosis5 have been described. We present a rare case of Mycobacterium branderi diagnosed by cryoEBUS.
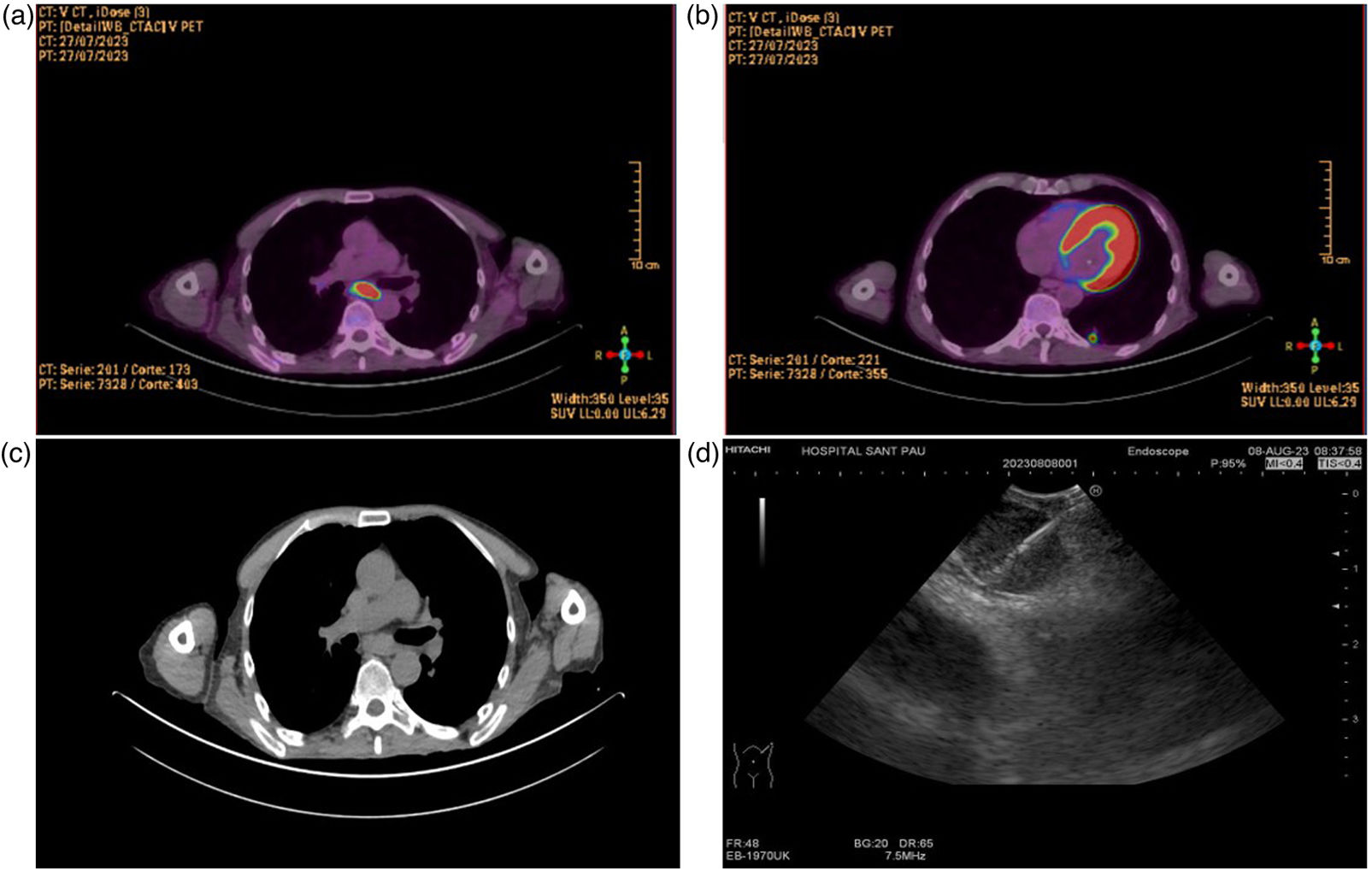
A 57-year-old male ex-smoker, with human immunodeficiency virus (HIV) infection without active treatment by their own decision presented to a hospital because of weakness and weight loss. Blood culture and virus test were negatives and chest X-ray showed no apparent lesions. A cranial CT and lumbar puncture ruled out infection. A positron emission tomography/computed tomography (PET/CT) showed a hypermetabolic pulmonary nodule (14mm, SUVmax 6.76) in left lower low (LLL) and enlarged mediastinal lymphadenopathies (subcarinal 25mm, SUVmax 19.03) (Fig. 1). EBUS-TBNA (EB-1970UK, Linear-Array; Pentax Medical Company) was performed under general anaesthesia by an anaesthesiologist using intravenous midazolam, propofol and fentanyl. With a 22-gauge needle (ECHO-HD-22-EBUS-O, Cook Medical Company), we performed two punctures and obtained cytological samples and cell blocks, evaluated by rapid on-site evaluation (ROSE). Then procedure with 22-gauge histological needle (ECHO-HD-22-EBUS-O-C), and after two punctures, a cryoEBUS was performed in subcarinal region, introducing a 1.1mm cryo-probe (Erbecryo 20402-401, Tubingen, Germany), obtaining three cryobiopsies (Fig. 1). The procedure was well tolerated and no complications were observed, nor 72h later. Cytological studies showed lymphocytes without malignant cells from either the punctures or the cell block. The cultures did not show germs, and the polymerase chain reaction (PCR) and mycobacteria's culture were negatives. Finally, in cryoEBUS culture grows M. branderi and patient was referred to infectious unit for assessment.
To the best of our knowledge, is the first case of atypical mycobacteria diagnosed by cryoEBUS. CryoEBUS is a new and safe procedure,2–4 that could represent a promising technique in the study of intrathoracic lymphadenopathy.2 The overall diagnostic yield described is about 91.8% for cryoEBUS3 and seems more sensitive in uncommon tumours and benign disorders.
The poor tissue representation of EBUS-TBNA samples might restrict the diagnostic yield for certain conditions such as lymphoproliferative and granulomatous disorders,4 and cryobiopsy samples have demonstrated to be architecturally better preserved and bigger in size.2,4 In our case, EBUS-TBNA did not allow establishing the final diagnosis and definitive microbiological diagnosis was achieved by cryobiopsy. Diagnostic yield for EBUS-TBNA in the diagnosis of mycobacterial diseases such as tuberculosis is around 80%,5 and cryoEBUS has been shown to significantly increase the efficacy to above 90%2 but there are no references about non-tuberculous mycobacteria.
In conclusion, cryoEBUS is a safe and feasible technique in expert units, that offer a high diagnostic yield and could be a new option for infection diagnosis, thereby improving the diagnostic strategy for non-malignant diseases. More clinical studies are needed.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ ContributionsAll authors have contributed substantially to obtaining the results and preparation of the manuscript, according with ICMJE criteria.
Conflicts of InterestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.
Artificial Intelligence InvolvementArticle was produced without the help of any artificial intelligence software or tool.