Pulmonary embolism (PE) is a common lung disorder, but it is difficult to diagnose and is confirmed using objective tests in only 20% of patients.1 Furthermore, there is no single test that is sufficiently sensitive or specific for diagnosis in all cases.2 The primary indication for endobronchial ultrasound (EBUS) is the aspiration of mediastinal adenopathies and central masses for cancer diagnosis and staging. However, the 2–5cm depth of field of the ultrasound bronchoscope allows the pulmonary artery trunk, main pulmonary arteries and lobar arteries to be visualized. We describe a case of PE in which the first diagnostic technique used was endobronchial ultrasound.
A 52-year-old woman, an active smoker with a cumulative rate of 20 pack-years was referred from her primary care physician after the discovery of multiple bilateral nodules, a left hilar mass and pericardial effusion. She reported a 3-month history of cough with whitish expectoration, and dyspnea on moderate exertion for the previous month and a half. She also complained of an episode of erythema, edema, heat and pain in the distal part of the left lower limb over the previous 15 days, which resolved without treatment.
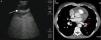
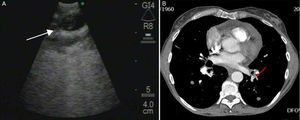
A bronchoscopy was performed in which no endobronchial abnormalities were observed. Using EBUS (BF-UC160F Olympus, Japan), adenopathies in areas 4R (0.48cm), 4L (0.75cm) and 7 (0.60cm) were aspirated, and an echogenic intraluminal image was incidentally observed in a branch of the left lower lobe artery (Fig. 1). Laboratory tests revealed d-dimer 8140ng/ml. The electrocardiogram was normal but signs of thrombophlebitis were observed in the distal area of the left lower limb on Doppler ultrasound. The presence of PE in the posterior segmental arteries of both lower lobes was confirmed by computed tomography angiography (angio-CT). The final diagnosis was lung cancer, stage T2 N3 M1a.
Although the role of EBUS in the diagnosis of PE has still not been established, it may be useful in some hemodynamically stable patients in whom other techniques cannot be performed. According to the PIOPED II study, angio-CT is contraindicated in 24% of patients with PE,3 including advanced renal failure and pregnancy. In addition, magnetic resonance angiography cannot be performed in patients with metal implants, such as pacemakers. Another advantage of EBUS is that it can be carried out in the intensive care unit, thereby avoiding complex patient transfers. Finally, EBUS easily allows malignant vascular diseases to be differentiated from PE, obviating the need for diagnostic surgical procedures.
Most cases of PE diagnosed by EBUS have described patients with filling defects in central arteries previously detected by another imaging technique. However, in this patient, EBUS was the first diagnostic technique used, showing good correlation with the findings on the subsequent angio-CT.4,5 Our case demonstrates the usefulness of EBUS as an initial technique for the diagnosis of PE, not only in central arteries, but also in more peripheral branches.
Please cite this article as: Llopis Pastor E, et al. Tromboembolismo pulmonar diagnosticado mediante ecobroncoscopia. Arch Bronconeumol. 2013;49:555–556.