Pulmonary foreign body granulomatosis is a rare condition where a granulomatous inflammation reaction to foreign bodies occurs in the lungs.1 It is usually secondary to intravenous injection of pulverized pharmaceutical tablets or by nasal inhalation of drugs containing insoluble binders.2
Cosmetic dermal fillers can also produce a foreign body reaction of the skin with multinucleated giant cells that can happen weeks or years after the injection of a cosmetic filler.3 Its clinical incidence has been reported to range from 0.02% to 1%.4
We report a case of a female patient with 66 years old, ex-smoker (50 pack-years), with a history of bilateral recurrent uveitis, Parkinson's disease, depression, alcoholism and multiple plastic surgeries. She had had a cosmetic dermal filler facial injection in 1994.
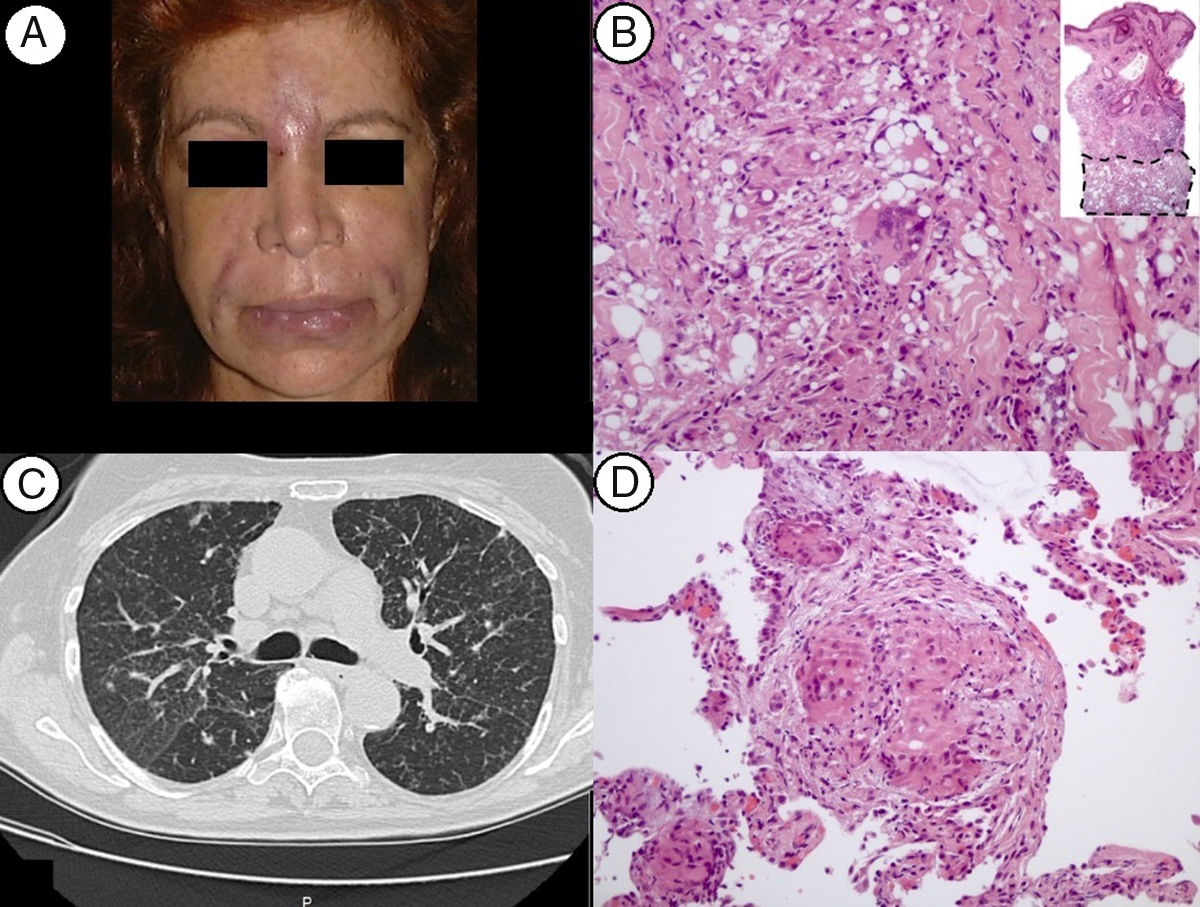
Respiratory symptoms appeared after an episode of facial cellulites for which the patient was admitted to the Dermatology nursery. She presented with erythema and edema of the face, with tender areas at the inter-ciliary region and naso-genian sulc (Fig. 1A). Biopsies of these areas were suggestive of granulomatous reaction foreign body-like associated with lipidic material (lipogranulomas). She was first treated with antibiotics, topical injection of 5-fluoracil and betamethasone with only partial improvement and the need for surgical debridement. Histological exam of the excised lesion showed chronic inflammatory reaction with multiple lymphocytes, epithelioid histiocytes and small rare granulomas with giant multinucleated cells, associated with round multisized vacuoles, predominantly extracellular and non-refringent (Fig. 1B). These changes were interpreted as foreign body granulomatous reaction to the cosmetic dermal filler injected 11 years earlier.
(A) Patient with erythema and edema at the inter-ciliary region and naso-genian sulc; (B) the skin biopsy revealed a deep and severe inflammatory process, depicting lipogranulomas with multinucleated giant cells of the foreign body type (H&E, 40× and 200×); (C) HRCT-L showing a micronodular milliary pattern of the upper lobes, ground glass areas and slight thickening of interlobular septae; (D) microphotograph of the lung biopsy showing sarcoid-like epithelioid granulomas with multinucleated giant cells of the foreign body type (H&E, 200×).
She was first evaluated at the pulmonology clinic in 2005 for a 6 month history of productive cough, dyspnea, pleuritic right chest pain and weight loss of 8kg.
High resolution computerized tomography of the lungs (HRCT-L) showed mediastinal adenopathies and a micronodular milliary pattern of the upper lobes with ground glass areas (Fig. 1C) as well as interstitial fibrosis at the lower lobes. Functional respiratory assessment showed air trapping (RV 145%) and reduced DLCO (DLCO 42%, DLCO/VA 59%). Auto-immune blood tests, angiotensin conversion enzyme and HIV, HBV and HCV serologies were negative. Broncho-alveolar lavage was lymphocyte predominant (44%, CD4:CD8=14) and bacteriological, mycological and microbacteriological exams were negative. Transbronchial biopsies revealed non necrotizing granulomas with a vasculocentric distribution and with giant multinucleated cells foreign body like (Fig. 1D).
The hypothesis of lung granulomatous disease secondary to the injection of a cosmetic dermal filler was admitted. The patient was started on prednisolone and azatioprin, with clinical improvement. Azatioprin was stopped in 2012 and prednisolone in 2013. The patient was not compliant to the regular follow up at the pulmonology clinic and she was later re-evaluated in 2016. DLCO had further decreased (31%) and she maintained mediastinal adenopathies, coalescent micronodules of the upper lobes, bronchiectasis and fibrosis. Prednisolone was started again (20mg/day) and the patient was referred to the interstitial lung disease clinic. Case was discussed at the multidisciplinary meeting. The diagnosis previously considered was accepted and immunosuppression was maintained.
Cosmetic dermal fillers can be classified as resorbable fillers (such as collagen or hyaluronic acid) or permanent/nonreasorbable fillers (such as silicone).3 Ideally they should be biocompatible and they should induce minimum foreign body reaction.4
Foreign body reaction occurs when large foreign bodies cannot be phagocytosed by macrophages triggering aggregation of macrophages into multinucleated giant cells and formation of granulomas. There are different types of foreign body granulomas with different clinical and histologic features (cystic granulomas, lipogranulomas and sclerosing granulomas) depending on the type of filler used. However mixed type granulomas can also occur. Cystic granulomas are composed of giant cells and macrophages and usually occur with the injection of hyaluronic acid or collagen. Lipogranulomas occur mainly with the injection of silicone, paraffin or polyacrylamide gels and they have variously sized vacuoles, macrophages, and giant cells. Finally sclerosing granulomas (appearing usually with the injection of polymethylmethacrylate microspheres or polylactic acid microspheres) are made of empty vacuoles with even sizes and shapes, and the spaces between the vacuoles are filled with multinucleated giant cells, macrophages, fibroblasts, and collagen fibers produced by fibroblasts.3
One of the most probable causes for non-infectious granulomatous lung disease, sarcoidosis, remains without a known cause. It is thought that sarcoidosis occurs when a patient with genetic susceptibility to the disease is exposed to a specific environmental antigen. According to Marcoval et al.,5 the immune system's capacity of sarcoidosis patients to handle foreign matter is compromised and the presence of foreign bodies in the skin might provide the stimulus necessary to granuloma formation. However it is still uncertain if the presence of polarizable foreign material within sarcoidal granulomas is compatible with the diagnosis of sarcoidosis.6,7
The injection of a cosmetic dermal filler normally induces a weak granulomatous reaction which can be exacerbated by interferon and other immunostimulatory medications triggering systemic sarcoidosis.6 Our patient, however, was not exposed to any of those medications.
In conclusion pulmonary involvement following skin granulomatous reaction to foreign bodies is not frequent8 and pathophysiology is not totally understood. In our patient a larger lung biopsy could have confirmed the presence of lipogranulomas or foreign body material and strengthened the diagnosis. However the case was discussed in our interstitial lung disease multidisciplinary meeting and that was the accepted diagnosis. To our knowledge, this is the first case of granulomatous lung disease manifesting after cutaneous granulomatous reaction secondary to the injection of a cosmetic dermal filler.