Home oxygen therapy (HOT) improves survival in patients with chronic obstructive pulmonary disease (COPD) and severe respiratory failure.1 The prevalence of HOT has increased in recent decades, leading to an increase in costs.2,3 This intervention should be indicated in non-smoking patients in a stable phase who meet the established criteria for HOT and who are receiving optimal drug therapy. Arterial blood gas should be determined at rest and in a sitting position.4 If HOT is prescribed in the acute phase, as often occurs after a hospital admission,5 it is important that it is subsequently evaluated when the patient is stable, in order to avoid inefficient use,6 since it has been demonstrated that in many cases, HOT may be withdrawn.7–9 Unnecessary HOT can also be a burden for patients, and has been associated with feelings of discomfort, restrictions in daily activities, and social isolation, contributing to poor compliance.10 In our hospital, we have a dedicated oxygen therapy clinic where all provisional prescriptions are reviewed within approximately 3 months. The aim of this study was to analyze the progress of patients who were withdrawn from HOT, and to study the characteristics of those in whom it was restarted, a topic not addressed previously in the literature.
Between October 2015 and August 2017, 960 provisional prescriptions for oxygen therapy were made, of which 483 were withdrawn. These patients were followed for 1 year and the impact of HOT withdrawal was analyzed, taking into account the need for restart, hospital readmissions for cardiorespiratory reasons, and mortality. The characteristics of patients who required restart of HOT were also studied. After a descriptive analysis of patients, COPD patients in whom HOT was restarted were compared to those in whom it was not (Chi-squared test for qualitative variables, Student’s t-test for age and FEV1, and the Mann–Whitney U test for pO2 determined in the clinic at the time of withdrawal). We also evaluated if HOT was restarted correctly or incorrectly, and conducted a logistic regression multivariate analysis to study the factors that were associated with restarting HOT in these patients. A p value < 0.05 was considered statistically significant. The SPSS® package version 20.0 was used for the statistical analysis.
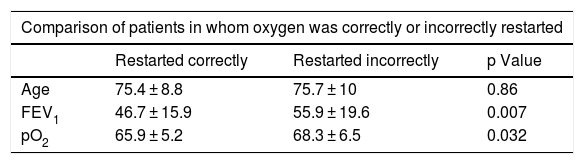
Mean age of the 483 patients was 77.6 ± 10 years and 59% were men. Ninety percent of the prescriptions were made at the time of hospital discharge. The most common diseases were: COPD (40.5% of cases), pneumonia (20.5%), heart disease (14%), and asthma (10%). Mean pO2 at the time of withdrawal of HOT was 69.4 ± 7 mmHg. In the first year after withdrawal, HOT was restarted on a provisional basis in 99 patients (21%), albeit incorrectly in 44 (43.5%), either due to failure to determine arterial blood gases at the time of the prescription, or because the patients did not meet the criteria for oxygen therapy.4 Thirty-three percent of patients in whom HOT was restarted incorrectly had previously documented hypercapnia. Of the 55 patients in whom HOT was restarted correctly, 36 (65.5%) were diagnosed with COPD (mean FEV1 46.4% ± 16%), and 75% were readmitted for exacerbations. Mean time to restart of HOT was 7 ± 4 months. COPD patients in whom HOT was correctly restarted had lower FEV1: 46.7 ± 15.9 (p < 0.007), pO2: 65.9 ± 5.2 (p < 0.032) and a greater number of hospitalizations (p < 0.0001) than the others. In the multivariate analysis, the restart of HOT was associated with a greater number of hospitalizations subsequent to withdrawal (Table 1), because HOT is often used to facilitate discharge home and reduce length of hospital stay. Of patients who were withdrawn from HOT during the follow-up period, 156 (33%) were admitted for cardiorespiratory causes, within a mean time of 6.2 ± 3.4 months. Seventy-nine patients (17%) died, the most frequent causes being respiratory (19 patients; 24%) and cardiac (14 patients; 18%). Mean time to death was 6.7 ± 3.7 months. Ten patients died in the first month: 1 in a traffic accident, 1 due to acute pulmonary edema, 2 of gastrointestinal bleeding, 1 due to stroke, and 1 due to cancer of the larynx, and 4 deaths occurred for unknown causes (death outside the hospital).
Comparison of the characteristics of patients in whom oxygen therapy was correctly or incorrectly restarted and factors associated with restarting oxygen in COPD patients (multivariate analysis).
| Comparison of patients in whom oxygen was correctly or incorrectly restarted | |||
|---|---|---|---|
| Restarted correctly | Restarted incorrectly | p Value | |
| Age | 75.4 ± 8.8 | 75.7 ± 10 | 0.86 |
| FEV1 | 46.7 ± 15.9 | 55.9 ± 19.6 | 0.007 |
| pO2 | 65.9 ± 5.2 | 68.3 ± 6.5 | 0.032 |
| Factors associated with restarting oxygen in COPD patients (multivariate analysis) | |||
|---|---|---|---|
| OR | 95% CI | p Value | |
| Age | 1 | (0.95–1.05) | 0.99 |
| FEV1 | 0.97 | (0.95–1.00) | 0.072 |
| pO2 | 0.97 | (0.90–1.04) | 0.46 |
| Subsequent admission | 5.46 | (2.26–13.13) | 0.00 |
95% CI: 95% confidence interval; COPD: chronic obstructive pulmonary disease; FEV1: forced expiratory volume in 1 s; OR: odds ratio; pO2: partial pressure of oxygen.
Our results seem to confirm that withdrawal of HOT is safe in patients who do not meet criteria for this treatment. However, COPD patients with severe exacerbations will require close monitoring, and respiratory day hospitals can be useful for this purpose.11
Oxygen therapy clinics, by correctly applying the criteria for indicating this intervention, have managed to significantly reduce the prevalence of HOT.5,7,8 Most prescriptions are made in the acute phase, and often do not follow the established recommendations.8,9,12 It is important to note that 33% of patients in whom HOT was incorrectly restarted had hypercapnia at the time of withdrawal. Administering oxygen to these patients can worsen hypercapnia and cause respiratory acidosis,13 as arterial pO2 levels play an essential role in the control of ventilation.14
COPD exacerbations are more frequent and severe as the disease progresses, and the risk factors for a new admission are FEV1 < 50%, previous hospitalizations, and use of HOT,15 characteristics that are in line with those of our study.
In summary, the withdrawal of HOT in patients who do not meet the indication appears safe, since it only has to be restarted in a small percentage of patients, nearly half of which do not meet the criteria for restarting HOT. COPD patients with exacerbations and severe airflow obstruction must be closely monitored. However, more studies are needed to analyze this highly prevalent problem.
Please cite this article as: Lourido-Cebreiro T, et al. Evolución tras la retirada de la oxigenoterapia domiciliaria. Perfil del paciente en el que hay que reintroducirla. Arch Bronconeumol. 2019;55:663–665.