Sarcomas are mesenchymal tumors that originate from the stromal elements of the bronchial wall or from interstices of lung parenchyma. Pulmonary sarcomatous neoplasms are a rare and diagnostically challenging group of tumors. They constitute only 0.2%–0.5% of all primary lung malignancies. Primary pulmonary leiomyosarcomas are subdivided into those originating from pulmonary parenchyma, bronchial tree or pulmonary arteries. Here we present a case of 43-year-old African-American female with chronic cough, fatigue and weight loss. Early detection is the key to the successful management of these patients. The available treatment option is complete resection of tumor. These cases provide an interesting juxtaposition to the management of typical lung cancer.
Los sarcomas son tumores mesenquimatosos que tienen su origen en los componentes de estroma de la pared bronquial o en el intersticio del parénquima pulmonar. Las neoplasias sarcomatosas pulmonares son un grupo de tumores muy poco frecuentes y difíciles de diagnosticar. Constituyen tan solo el 0,2-0,5% del total de enfermedades malignas primarias del pulmón. Los leiomiosarcomas pulmonares primarios se subdividen en los que se originan en el parénquima pulmonar, los derivados del árbol bronquial y los que proceden de arterias pulmonares. Presentamos aquí el caso de una mujer afroamericana de 43 años que presentaba tos crónica, fatiga y pérdida de peso. La detección temprana es la clave del tratamiento eficaz de estos pacientes. La opción de tratamiento existente es la resección completa del tumor. Estos casos proporcionan una yuxtaposición interesante con el tratamiento del cáncer de pulmón habitual.
A 43-year-old African-American female, with a known history of hypertension and osteoarthritis of the right knee, came to our consultation complaining of cough and whitish sputum during the previous month. These symptoms had been accompanied by respiratory difficulty for the previous 2 weeks, which had progressively increased and was more pronounced when climbing stairs or walking a few meters. The patient denied having nausea, vomiting, diarrhea or loss of appetite, but had noticed a weight loss of 4.6kg over the course of the last 3 months. She was a never-smoker but had been exposed to the prolonged second-hand smoke of her husband. Her surgical history included oophorectomy and hysterectomy 8 years before due to a dermoid cyst and multiple uterine fibroids, which were confirmed to be benign by biopsy. Upon exploration, we observed that the patient presented with clubbing, deviation of the trachea to the left and notably reduced respiratory sounds in all the right pulmonary fields, with dullness to percussion. There was increased vocal fremitus and resonance, with egophony. The hematological and biochemical analyses were normal.
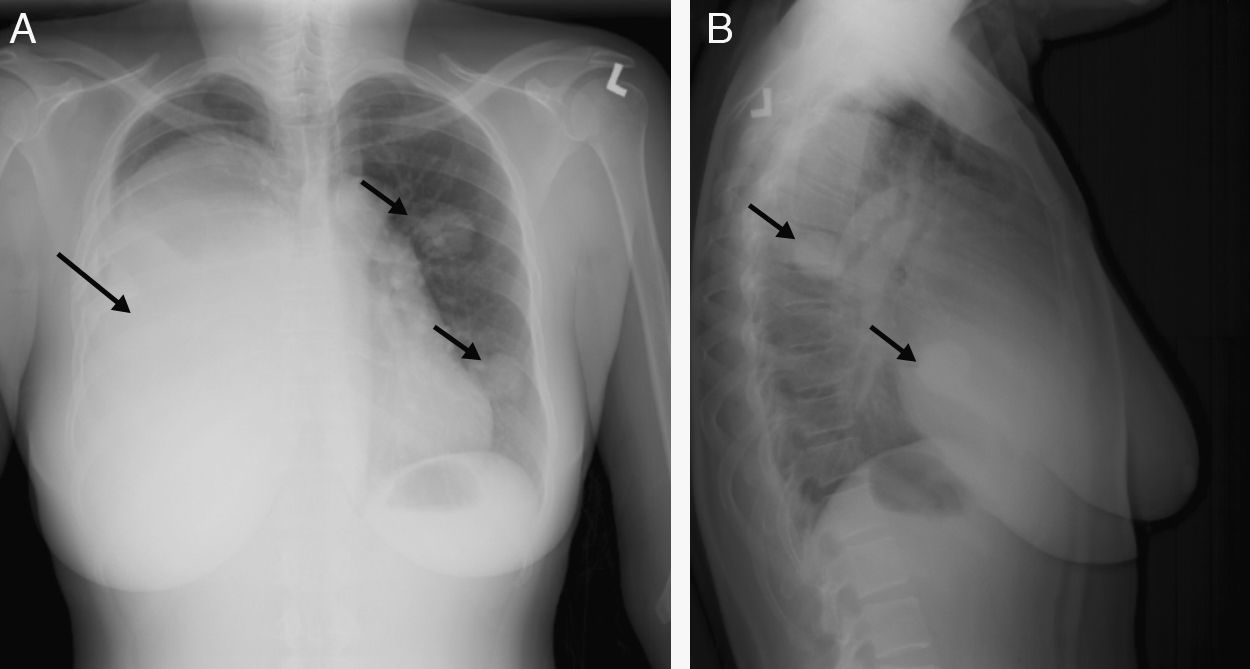
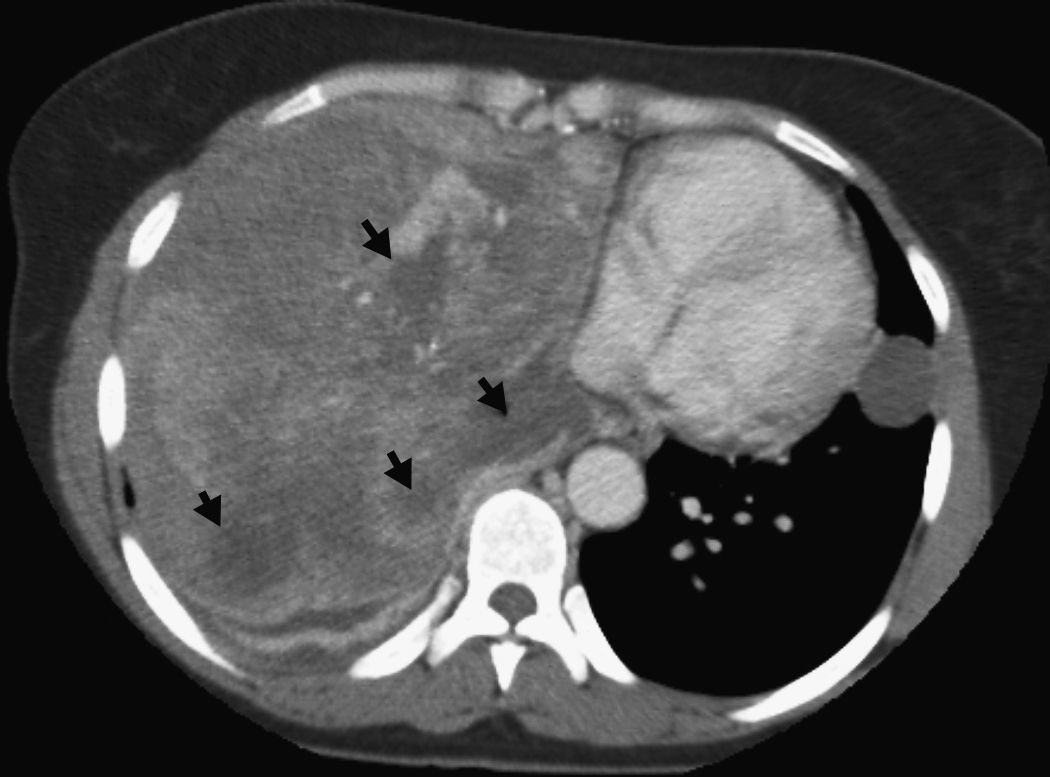
Imaging tests were ordered and chest radiography (Fig. 1A and B, arrows) showed a homogenous opacity on the right side that affected most of the right lung, with pleural effusion, deviation of the trachea toward the left and two coin-shaped opacities in the left lung field (arrows). An additional imaging test, chest computed tomography (CT) (Fig. 2), revealed the presence of a large heterogeneous mass with multiple foci of necrosis (arrow tips) and collapse of the right lung. The two coin-shaped lesions observed on the chest radiograph in the left lung were confirmed by CT. The mediastinum was deviated toward the left, with no significant lymphadenopathies.
Later, the diagnostic pleural puncture revealed the presence of a serosanguinous fluid with lymphocytes and mesothelial cells. No malignant cells were isolated. Gram and Zeil–Nielsen stains were negative. Diagnostic studies were carried out in order to rule out the possible presence of a primary tumor somewhere else by means of abdominal, pelvic and cranial CT, and mammography. All the tests were normal.
On the fifth day, CT-guided biopsy of the right lung mass revealed fragments of a neoplasm of fusiform cells with epithelioid characteristics. Immunohistochemical staining showed intense reactivity with desmin, smooth muscle actin (SMA) and caldesmon, which supports differentiation of smooth muscle. A diagnosis was established of primary pulmonary leiomyosarcoma with metastasis in the contralateral lung. The patient requested to be transferred to a specialized oncologic center, where she underwent right pneumonectomy and was administered palliative chemotherapy and radiotherapy.
DiscussionPrimary pulmonary sarcoma (PPS) are exceptionally rare tumors that constitute only 0.2%–0.5% of all lung cancers.1,2 Pulmonary leiomyosarcoma is the most common pathological type.1 Leiomyosarcoma of the lungs may originate in the arteriolar walls, muscle tissue in the interstitial plane of the alveolar walls or in primitive mesenchymal cells. Pulmonary sarcomas are fundamentally metastatic in etiology. Consequently, it is necessary to rule out metastatic extrapulmonary sarcomas as well as sarcomatoid carcinomas before establishing a diagnosis of PPS. The patients usually present with unspecific symptoms, and therefore early diagnosis is difficult. It is frequent that the form of presentation is a round, well-outlined mass on chest radiography. Unlike epithelial tumors, these tumors do not show a tendency to exfoliate and, therefore, bronchoscopy is not an appropriate diagnostic method.3 Leiomyosarcomas spread through the bloodstream and, although infrequently, through the lymph vessels, making mediastinoscopy inappropriate for its diagnosis. The analysis of the pleural liquid may not provide much information for this same reason. It is characteristic for metastasis to occur later on in the process of the disease, which emphasizes the importance of early detection.
Primary pulmonary sarcomas are classified according to the cell of origin. They arise in the hilum and organize in the peribronchial smooth muscle fibers. Unlike other sarcomas that invade the bronchial tree, they expand locally in the parenchyma, and the form of clinical, radiographic and macroscopic presentation of these very rare lung tumors does not significantly differ from that of more common lung tumors. For precise identification and classification, it is necessary to obtain complete samples and perform a detailed microscopic examination, as well as immunohistochemical and molecular analyses.4 Given the fact that pulmonary metastases of extrapulmonary sarcomas are more frequent than primary lung affectation, the basic diagnostic difficulty lies in ruling out a secondary origin of the sarcoma. CT and magnetic resonance currently play an important role in determining the extension of the invasion of primary thoracic sarcoma, possibilities for extirpation and response to treatment. However, ultimately an anatomic pathology evaluation is necessary to precisely establish the diagnosis.5 The histologic diagnosis of leiomyosarcoma is suspected when a fascicular proliferation of fusiform cells that show intersections at right angles is identified. It is characteristic for tumor cells to have a limited fibrillar eosinophilic cytoplasm and large nuclei.6 The histologic impression for differentiating the smooth muscle itself may be confirmed by means of a battery of immunohistochemical markers, such as desmin, smooth muscle actin and caldesmon. Other tumors to keep in mind in the differential diagnosis are the following: non-differentiated carcinoma, biphasic tumor, carcinosarcoma, carcinoid tumor, intrapulmonary thymoma and lymphoma.
Applicable therapeutic methods include surgical resection, which, if complete, is usually curative for small and well-differentiated sarcomas. Radical surgical extirpation is generally the optimal treatment. Poorly differentiated and non-resectable tumors can be treated with palliative radiotherapy or chemotherapy. Median survival is 48 months, and the 5-year survival rate ranges between 38% and 48%.5 Other therapeutic methods include radiotherapy and adjuvant chemotherapy, but the results are not very satisfactory.
Primary pulmonary leiomyosarcoma is a very rare clinical-pathological disorder that requires early detection, an exhaustive diagnostic study and staging in order to decide on proper therapy and determine prognosis. Very little is known about its clinical-pathological variants. The most consistent predictive factor for long-term survival is the tumor stage. The size of the tumor, clinical stage and complete resection are variables to take into account. The best therapeutic method is surgical resection, but unfortunately only one-third of the cases can be treated surgically due to patient factors or the extension of the tumor.
Conflict of InterestsThe authors have no conflicts of interest to declare.
Please cite this article as: Luthra M, et al. Leiomiosarcoma pulmonar primario: presentación de un caso. Arch Bronconeumol. 2012;48:476–8.