Pneumoperitoneum is defined as the presence of air in the peritoneal cavity. In the absence of previous surgery, the most common cause, accounting for up to 90% of cases, is perforated hollow viscus.1 Nevertheless, pneumoperitoneum may also be caused by processes not requiring surgical treatment, in which case it is called benign, non-surgical, idiopathic or asymptomatic pneumoperitoneum. It can be triggered by multiple causes, one of which is the use of mechanical ventilation.1,2
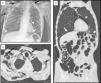
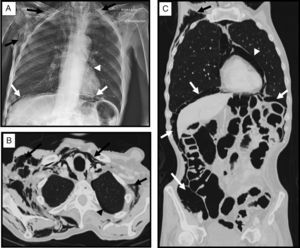
We report the case of a 73-year-old man who was referred to our center for PEG placement (gastrostomy), due to his inability to ingest solids and fluids. Personal history included amyotrophic lateral sclerosis (ALS) diagnosed 2 years previously, treated with non-invasive mechanical ventilation (NIMV) (VIVO 50, S/T mode, with face mask), with IPAP values in the last year of 24cm/H2O and EPAP 8cm/H2O. In the last week, the patient required longer ventilation times and could not tolerate disconnections. On physical examination he was breathing normally, with no respiratory difficulty, and curve patterns with the preset parameters were excellent. Vital signs were normal with 99% O2 saturation and a respiratory rate of 18bpm. Of particular note on examination was significant subcutaneous emphysema, mainly in the right hemithorax with no prior history of injury or surgery. A chest radiograph was performed, revealing extensive emphysema in the cervicothoracic subcutaneous tissue, pneumomediastinum and pneumoperitoneum (Fig. 1A). In view of the finding of pneumoperitoneum, a chest and abdominal computed tomography was performed with iodinated contrast, which revealed, in addition to the chest radiograph findings, minimal left apical pneumothorax; perforated hollow viscus was ruled out (Fig. 1B and C). Given the patient's good general status, the radiological findings, and the use of NIMV, it was decided that the pneumoperitoneum was a complication of NIMV. Conservative treatment was adopted with high flow oxygen therapy (4lpm), and reduction of IPAP to 20cm/H2O, with resolution of the atypical air in the chest radiograph at 7 days.
(A) Portable chest radiograph showing extensive subcutaneous tissue emphysema of the cervical and thoracic region (black arrows), with pneumomediastinum (arrow head) and pneumoperitoneum (white arrows). (B and C) Chest-abdominal computed tomography axial image and coronal plane reconstruction with lung window, showing, as in the chest radiograph, subcutaneous tissue emphysema dissecting the muscle planes of the cervicothoracic region (black arrows), minimal left apical laminar pneumothorax (black arrow head), pneumomediastinum (white arrow head), and moderate pneumoperitoneum (white arrows), with no evidence of perforated hollow viscus.
Pneumoperitoneum may be of oropharyngeal, thoracic, abdominal, or gynecological origin. When abdominal disease has been ruled out, the most common origin is thoracic, and it has been described in association with cardiopulmonary resuscitation maneuvers, parenchymal lung disease, pneumomediastinum, pneumothorax, closed chest injuries, and use of mechanical ventilation.1–3 Pneumoperitoneum caused by mechanical ventilation is a rare complication, the incidence of which is unknown, although it is estimated to occur in about 7% of patients receiving invasive ventilation.4 Risk factors include high airway pressure, increased tidal volume, pre-existing lung disease (obstructive airway disease and acute respiratory distress syndrome), and duration of time on mechanical ventilation.5
The unusual feature of our case is that pneumoperitoneum as a complication of NIMV is very rare, and occurs more frequently with invasive ventilation. A review of the MEDLINE index found reports of only 3 cases of pneumoperitoneum caused by NIMV.6–8 A fourth case was reminiscent of our patient: a patient with ALS receiving NIMV who developed pneumoperitoneum after PEG placement, in whom it was impossible to determine if the cause was the interventional procedure or the use of NIMV, or a combination of both.9 The physiopathological mechanism that causes barotrauma and the passage of air from the chest cavity into the abdomen was studied by Macklin et al., who performed experimental studies in animal models, showing that airway pressures higher than 40cm/H2O caused interstitial emphysema, pressures higher than 50cm/H2O caused mediastinal emphysema, and if pressures exceeded 60cm/H2O, subcutaneous emphysema and pneumoperitoneum developed.10 If excessive pressure is applied to the trachea, hyperinflated and over-expanded alveoli will rupture. The expanding extra-alveolar gas is forced down a pressure gradient toward the perivascular interstitium, causing interstitial emphysema. From the interstitium, air progresses along the bronchovascular sheath until it reaches the pulmonary hilum and the mediastinum. This causes pneumomediastinum that can extend into the subcutaneous tissue, giving rise to subcutaneous emphysema, or into the retroperitoneum, causing pneumoretroperitomeum, extending in a posterior direction toward the abdomen, crossing the mesentery or the foramen of Winslow. When air is applied at higher pressures, the alveoli rupture into the pleural space generating a pneumothorax that can extend to the abdominal cavity through small pleuroperitoneal anatomical defects, causing pneumoperitoneum.11 Hillman reviewed 28 cases of pneumoperitoneum in humans caused by mechanical ventilation and found that in most patients, inspiratory pressures exceeded 40cm/H2O and final expiration positive pressures were greater than 6cm/H2O.12 When using mechanical ventilation, IPAP values should not exceed 20cm/H2O and EPAP 6cm/H2O, since higher values are associated with barotrauma.13,14 Due to disease progression in our patient, inspiratory and expiratory positive pressures had to be increased to 24 and 8cm/H2O, respectively, after which he remained stable with no signs of barotrauma. These IPAP and EPAP values are slightly higher than the recommended ranges, and this, along with the impossibility of performing disconnections in the last week, leads us to believe that this was the factor that caused the pneumoperitoneum, since the patient had no signs of barotrauma during daily disconnections of up to 5h. Treatment depends on the clinical impact, and decompressive maneuvers are required in the case of tension pneumoperitoneum, in order to avoid abdominal compartment syndrome, although this tends to be unusual. This type of pneumoperitoneum generally has no clinical repercussions, and can be managed with conservative treatment or a wait-and-see approach,15 as in our case.
In conclusion, the presence of air in the abdominal cavity is normally due to perforated hollow viscus, but the clinical impact of these cases tends to be high. In patients without symptoms there are other causes such as mechanical ventilation, when a barotrauma mechanism leads to the presence of atypical air in the abdominal cavity. In these cases, it is important to correlate the patient's clinical history with the treatments received.
Please cite this article as: Sánchez García S, Sanz Díaz J, Rubio Solís D. Neumoperitoneo como complicación de ventilación mecánica no invasiva. Arch Bronconeumol. 2017;53:588–589.