Brucellosis, or Maltese fever, is a zoonosis that is prevalent in the Mediterranean regions and is endemic in our country.1 The disease is acquired fundamentally by consuming non-pasteurized milk and dairy products, such as cheese and cream.2 Rarely, the pathogen can invade the respiratory system through inhalation. After an incubation period of 2–4 weeks, the brucellosis causes non-specific symptoms like fever of up to 40°C, night sweats, anorexia, tiredness and weightloss.3 The serum tube agglutination or microplate agglutination with Rose Bengal is especially used as a rapid screening test method for mass screening. Conventional serum tube agglutination (Wright agglutination test) is one of the most common laboratory tests used to confirm the diagnosis.4 The definitive diagnosis can be obtained with the isolation of the pathogen through hemoculture and a culture of a bone marrow sample.
A 20-year-old male patient who had just enlisted with the army came to our consultation complaining of cough, expectoration, sharp pain in the left hemithorax, night sweats, anorexia, fever in waves and dyspnea evolving over the previous 10 days. He also reported a weight loss of 3kg in recent months. At the time, he had a fever of 38.4°C with a respiratory rate of 22/min. Thoracic auscultation revealed bilateral basilar inspiratory rales. Leukocyte count was 27,930/mm3 and sedimentation rate was 68mm/h. C-reactive protein was 141mg/dl.
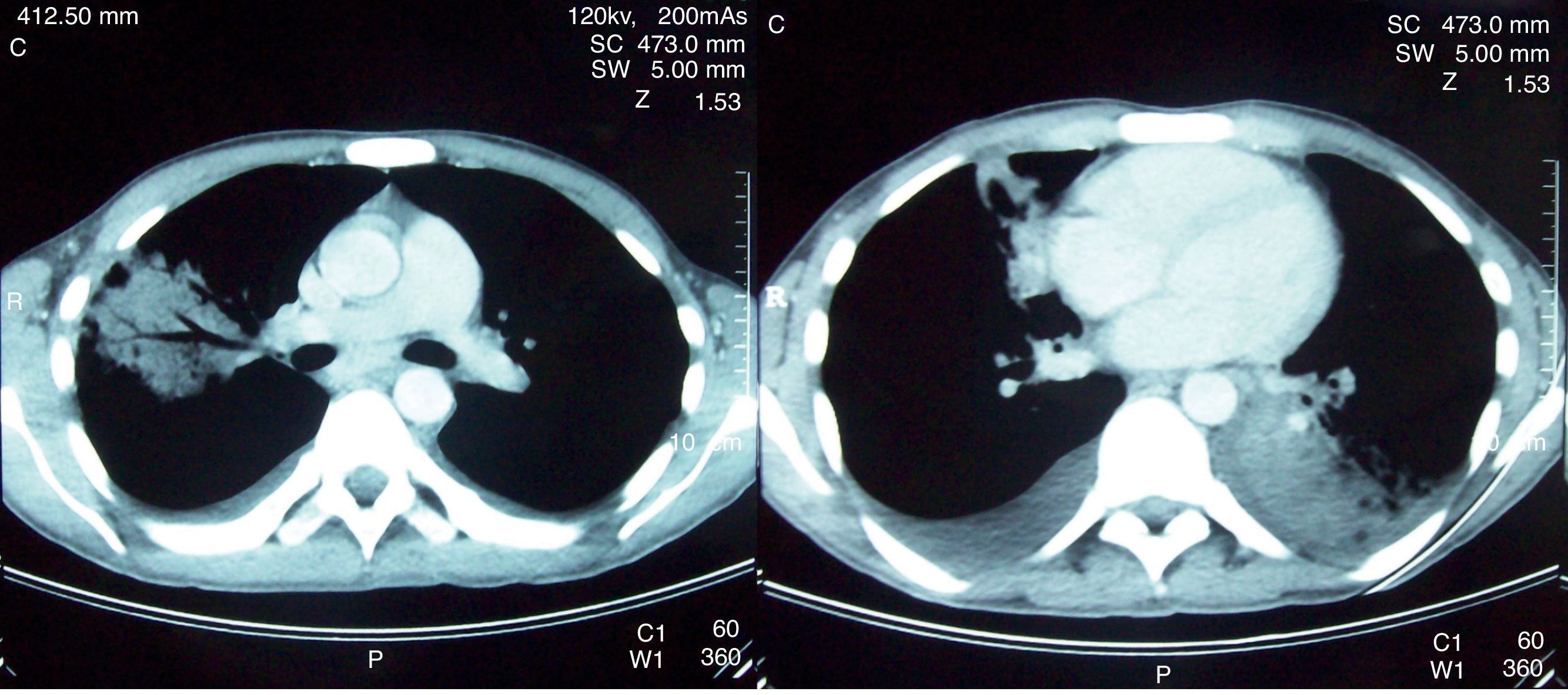
Chest radiography showed a pneumonic infiltrate in the right middle lobe and homogenous opacity in the left lower lobe. Computed tomography demonstrated bilateral pleural effusion of 2cm and pneumonic infiltrations in the anterior segment of the upper lobe and in the medial segment of the middle lobe of the right lung and in the lower lobe of the left lung (Fig. 1). The patient underwent thoracocentesis. The pleural liquid sample, which was straw-colored, was an exudate from a biochemical standpoint and contained 2000 leukocytes (80% mononuclear)/mm3. After the culture of the blood, urine and sputum samples were obtained, the patient was initiated empirical treatment with intravenous ampicillin-sulbactam at a dosage of 1g/day with a preliminary diagnosis of bacterial pneumonia and parapneumonic effusion. The sputum samples and pleural liquid were negative for acid-fast bacilli (AFB) and the level of adenosine deaminase in the pleural liquid was 31IU/l. In the sputum and pleural liquid cultures, no growth was observed.
On the sixth day of treatment, the patient continued to be feverish and there was no evident clinical or radiological improvement. Meanwhile, growth of Brucella spp. was documented in the hemoculture. When we took a more detailed personal history, it was revealed that the patient had lived in a village and worked as a shepherd, consuming non-pasteurized dairy products up until the month before. In addition, he reported that in his family there had been other cases of brucellosis. Serum agglutination with Rose Bengal was positive and the Wright serum agglutination was positive, with a titer of 1/160. The non-specific antibiotic therapy was interrupted on the sixth day and the patient initiated treatment with doxycycline at a dosage of 100mg 2 times a day and rifampicin at a dosage of 600mg/day orally. After 14 days of treatment, we saw an improvement in the clinical symptoms, radiological characteristics and the results of the arterial blood gases. The patient was released on the 20th day of hospitalization and he completed a 6-week treatment, making a complete recovery.
In a previous study done in our country, 1028 cases of brucellosis were retrospectively analyzed. 2% presented with cough, and in 7 patients (0.7%) there was pleural affectation.5 In a prospective study including 110 patients with brucellosis, in 11 (10%) there was lung affectation. It was documented that the treatment of the brucellosis led to complete remission of the pulmonary symptoms in all the cases, without other morbidities.6
In short, brucellosis can be confused with different diseases due to the lack of specificity of its clinical characteristics. Lung affectation is an uncommon manifestation, but it should be kept in mind in regions where the disease is endemic, especially if the patient does not respond to empirical antibiotic therapy.
Please cite this article: Berk S, et al. Neumonía y derrame pleural por Brucella. Arch Bronconeumol. 2012;48:301–2.