Mediastinal cavernous hemangioma (CH) is a rare benign vascular tumor of unknown etiology that presents more frequently in children and young adults.1 Pre-operative diagnosis by means of imaging tests is difficult and often cannot differentiate CH from a malignant solid tumor; therefore, we should consider the possibility of CH in patients with mediastinal tumors.
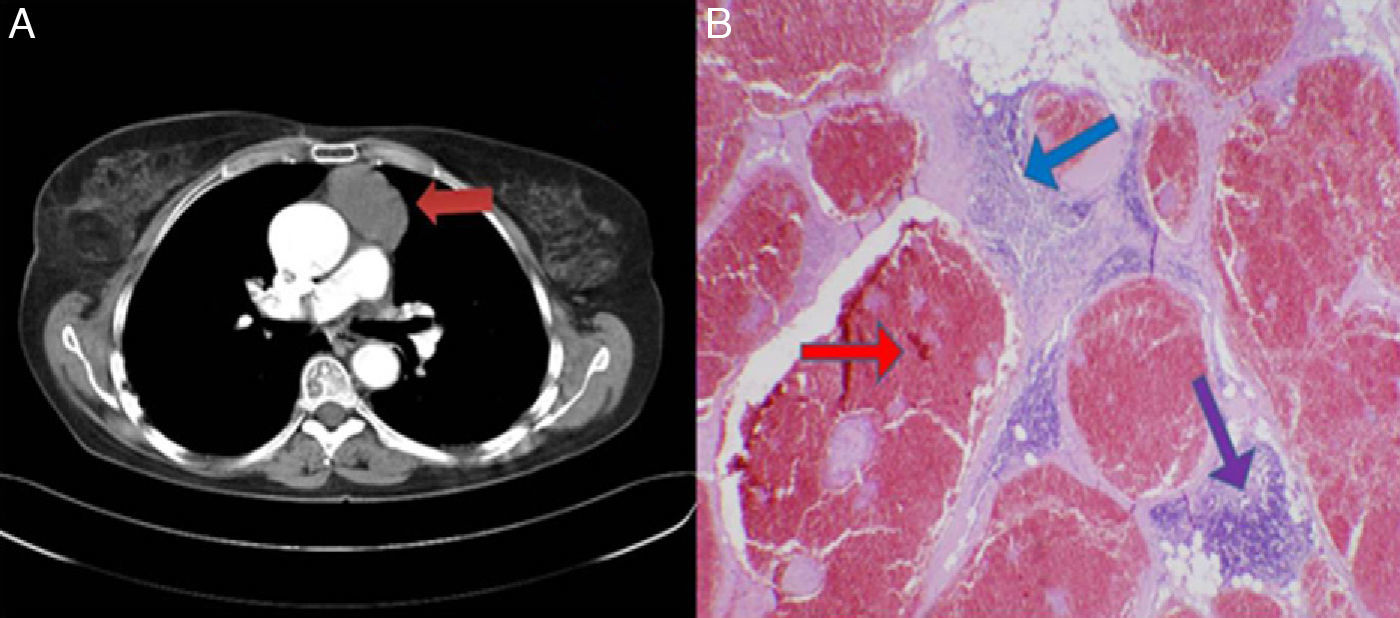
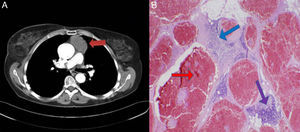
A 59-year-old woman, who underwent cephalic duodenopancreatectomy due to ampulla and tumorectomy in the right breast with axillary lymphadenectomy due to infiltrating ductal carcinoma, was referred to our department by the oncology unit after a coincidental finding on computed tomography (CT) of a mass in the anterior mediastinum measuring 5cm×4cm (Fig. 1A). We carried out complete analyses, arterial blood gases, spirometry, electrocardiogram, chest radiography and bronchoscopy, which were all normal. Surgical intervention was decided upon, proceeding with resection by means of mid-sternotomy of a very vascularized tumor in the perivascular area in close contact with the left pleura, with adequate surgical margins that included thymic tissue. The anatomopathologic study of the surgical piece revealed the presence of a thymic CH (Fig. 1B). The post-op period was free of complications and the patient presented no recurrences after 33 months of follow-up.
(A) The thoracoabdominal computed tomography shows the existence of a prevascular soft tissue mass (red arrow). (B) The anatomopathologic study of the surgical piece demonstrates dilated vascular channels full of blood and covered with flat endothelial cells without atypia (red arrow), fibrous septa that cross the lesion (blue arrow) and thymic tissue that is normal in appearance in the periphery (purple arrow), compatible with thymic cavernous hemangioma.
Almost 50% of mediastinal masses are located in the anterior mediastinum, the thymus being the most frequent origin.2 Thymoma is the neoplasm that most frequently affects the thymic parenchyma. It represents almost 10% of mediastinal masses3 and is normally benign but can be locally invasive and be confused with infrequent mediastinal vascular neoplasms like CH, making thymic CH more of a subsidiary of surgical treatment than other mediastinal hemangiomas.4 CH can be seen in any vascularized tissue and cause symptoms when infected or when they compress neighboring structures.5 Generally, the preoperative diagnosis of mediastinal hemangioma is difficult5 with imaging techniques. CH can show a characteristic enhancement after the administration of contrast in CT, and they are frequently associated with phlebolites on radiography; magnetic resonance imaging (MRI) shows a typical reticular appearance with a central area of mixed intensities and a hypointense rim in T2 that, however, may vary depending on the evolution time of the hemorrhages. Angiography is normal in 30%–40% of the patients, although it is useful for preoperative embolization. Angio-CT and angio-MRI are tests with ample resolution that can be very useful in the diagnosis of CH and in surgical planning. In the majority of cases described in the literature, the diagnosis of CH was confirmed by histologic study. It is necessary to carry out a differential diagnosis with other mediastinal vascular tumors, like angiolipoma, which is an uncommon benign tumor made up of adipose tissue and blood vessels, normally located in the subcutaneous cell tissue (although it may occasionally be found in other locations) and more frequently in children.
Asymptomatic CH usually does not require prophylactic treatment, as the morbidity and mortality associated with the hemorrhages caused by these lesions are relatively low, although once there has been an initial bleeding the rate of re-bleeding is relatively high. Surgical treatment in asymptomatic cases would be indicated if it is not possible to rule out malignant solid tumor due to doubts in the diagnosis. There have been reported cases of CH being resolved with thoracoscopy and video-assisted surgery.5
Relapses are directly related with incomplete resection. A meticulous, long clinical and radiological follow-up is recommended for early diagnosis of relapses.6
Please cite this article as: Roldán-Baños S, et al. Hemangioma cavernoso tímico. Arch Bronconeumol. 2012;48:303-4.