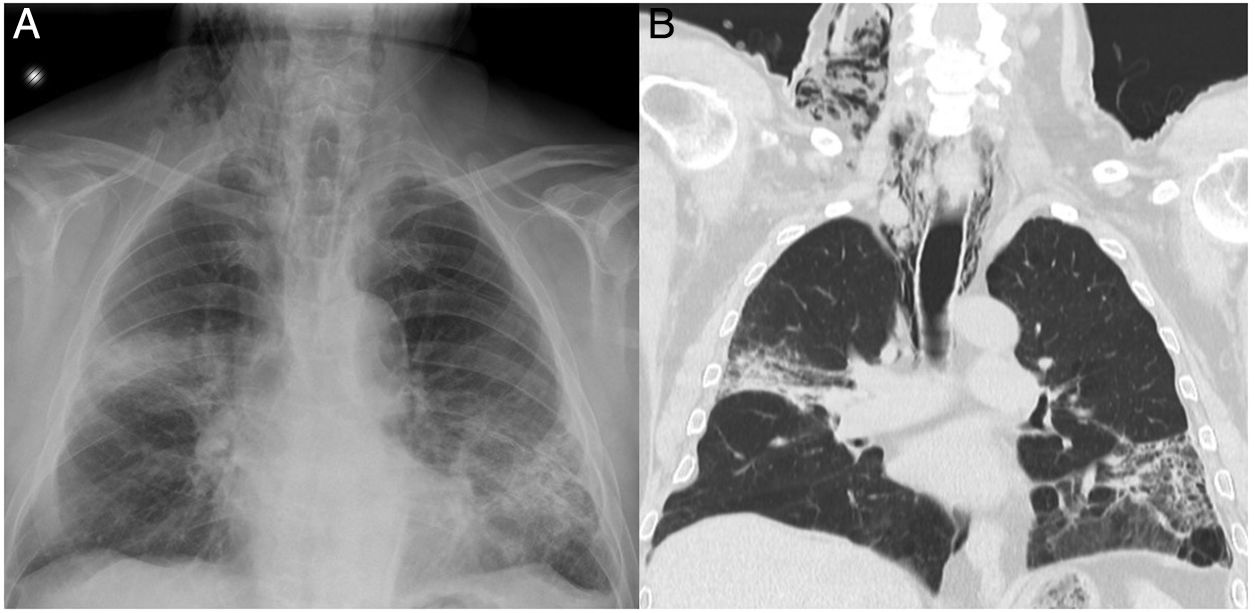
We report the case of an 82-year-old man referred to the respiratory medicine department with a 2-month history of dyspnea and desaturation, that did not improve with bronchodilator therapy. Chest X-ray showed bilateral lung consolidation, and chest computed tomography (CT) revealed areas of consolidation in right upper lobe (RUL) and left lower lobe (LUL) with associated reticulation. Given these findings, we decided to perform a fiberoptic bronchoscopy (FB) which showed diffuse endobronchial inflammation. Non-selective bronchial aspiration (BAS) and bronchoalveolar lavage (BAL) were performed during the procedure, without complications. Hours later, the patient reported an increase in his neck circumference. Chest X-ray showed subcutaneous emphysema (Fig. 1A) and an emergency CT showed pneumomediastinum (Fig. 1B). The patient was treated conservatively with analgesia and oxygen therapy, resulting in improved symptoms, so outpatient follow-up was recommended.
The origin of pneumomediastinum and subcutaneous emphysema can be spontaneous, traumatic, or iatrogenic. These complications have been described post-fiberoptic bronchoscopy in association with transbronchial biopsies.1 However, no cases have been described after simple fiberoptic bronchoscopy with BAS and BAL. The pathophysiologic mechanism of the process can be explained by the Macklin effect.2
Please cite this article as: Goicoechea Irigaray M, Rodríguez Alvarado I, Gómez Hernández MT. Neumomediastino y enfisema subcutáneo tras fibrobroncoscopia. Arch Bronconeumol. 2019;55:328.