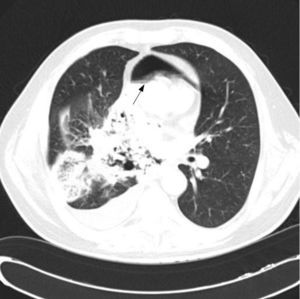
Documented cases of lung cancer complicated by pneumomediastinum and pneumopericardium are extremely rare. We report the case of a 55-year-old man with lung cancer complicated by pneumomediastinum and pneumopericardium. The patient was admitted with a 3-month history of dyspnea (Day 1). Computed tomography (CT) was performed and disease staging was established as cT4N3M0, although the tumor was not confirmed by histopathology. Pericardial and tracheal invasion were observed, causing tracheomediastinal fistula, pneumomediastinum (Fig. 1), and pneumopericardium. No distant metastases were observed. Bronchoscopy showed significant tumor stenosis on the trachea, approximately 6cm below the glottis. Samples could not be obtained and the procedure had to be terminated prematurely due to dyspnea.
The invasive bronchology team was consulted, but the conclusion was that bronchological intervention was impossible – at that time Y stents were not yet available in the hospital. The patient's condition deteriorated rapidly and he died on Day 10. Autopsy revealed squamous cell lung cancer with direct invasion of the pericardium and trachea, forming a tracheomediastinal fistula, pneumohydropericardium, left lung pneumonia (not present at the time of performing the CT). No distant metastases were observed, so stage pT4 and pM0 was confirmed (no information on N3 lymph node invasion was provided).
Only 4 cases of spontaneous pneumomediastinum in patients with primary lung cancer have been described.1–4 In 2 of them, the clinical situation deteriorated rapidly until death,1,2 1 patient recovered,3 and clinical progress was not reported in the fourth case.4 Histological types were large cell carcinoma,1 small cell carcinoma2,3 and undifferentiated carcinoma.4
There are 2 explanations for poor clinical progress in the cases discussed. Tracheomediastinal fistula carries a high risk for acute mediastinitis and possible development of tension pneumomediastinum. This, like tension pneumothorax, can rapidly be fatal.
We have identified 2 risk factors for the development of pneumomediastinum, both of which were presented by our case: direct tumor invasion of the trachea or the proximal ends of the main bronchi that can cause a leak to the mediastinum and raised airway pressure, occurring, for example, with intense cough or tracheal stenosis. Fistula formation does not appear to be associated with any specific histological type. Recommended treatment is symptomatic and includes high-flow oxygen therapy, analgesics and antibiotics. Preventive measures include treatment of the underlying cause of cough, if present, and endoscopic treatment of stenosis of the large airways. Tension pneumomediastinum is treated with decompression (incision or drainage).
To our knowledge, this is the first report of simultaneous spontaneous pneumomediastinum and spontaneous pneumopericardium in a patient with primary lung cancer. Our hypothesis is that, in this specific case, spontaneous pneumomediastinum was due to 2 circumstances: infiltration of the trachea (providing a less resistant area for fistula formation), and tracheal stenosis 6cm below the glottis (requiring a significantly greater change in intrathoracic pressure to maintain normal respiratory volume). Rapidly progressing respiratory failure was probably due to tracheal stenosis and pneumonia, rather than to spontaneous pneumomediastinum or spontaneous pneumopericardium.
Please cite this article as: Kara J, Klimesova S, Pauk N. Neumomediastino y neumopericardio en un paciente con cáncer de pulmón espinocelular. Arch Bronconeumol. 2015;51:249–250.