Idiopathic upper lobe fibrosis was described in 19921 and characterized by elastotic fibrosis in pleura and subpleural lung parenchyma, with a predilection for the upper lobes. In 2004 Frankel et al.2 applied the term pleuroparenchymal fibroelastosis (PPFE) for the first time, highlighting the pathologic findings of the disease. The latest update of international multidisciplinary classification of idiopathic interstitial pneumonia3 (IIP) includes PPFE in the section of rare IIP. Despite the initial thought that it represented a specific entity, current literature suggests that PPFE may likely represent a much more common form of chronic lung injury,4 associated with a variety of clinicopathologic conditions, such as infections, drugs, transplantation, autoimmune and interstitial lung diseases. We report a case of silicosis and PPFE, a possible association not yet established.
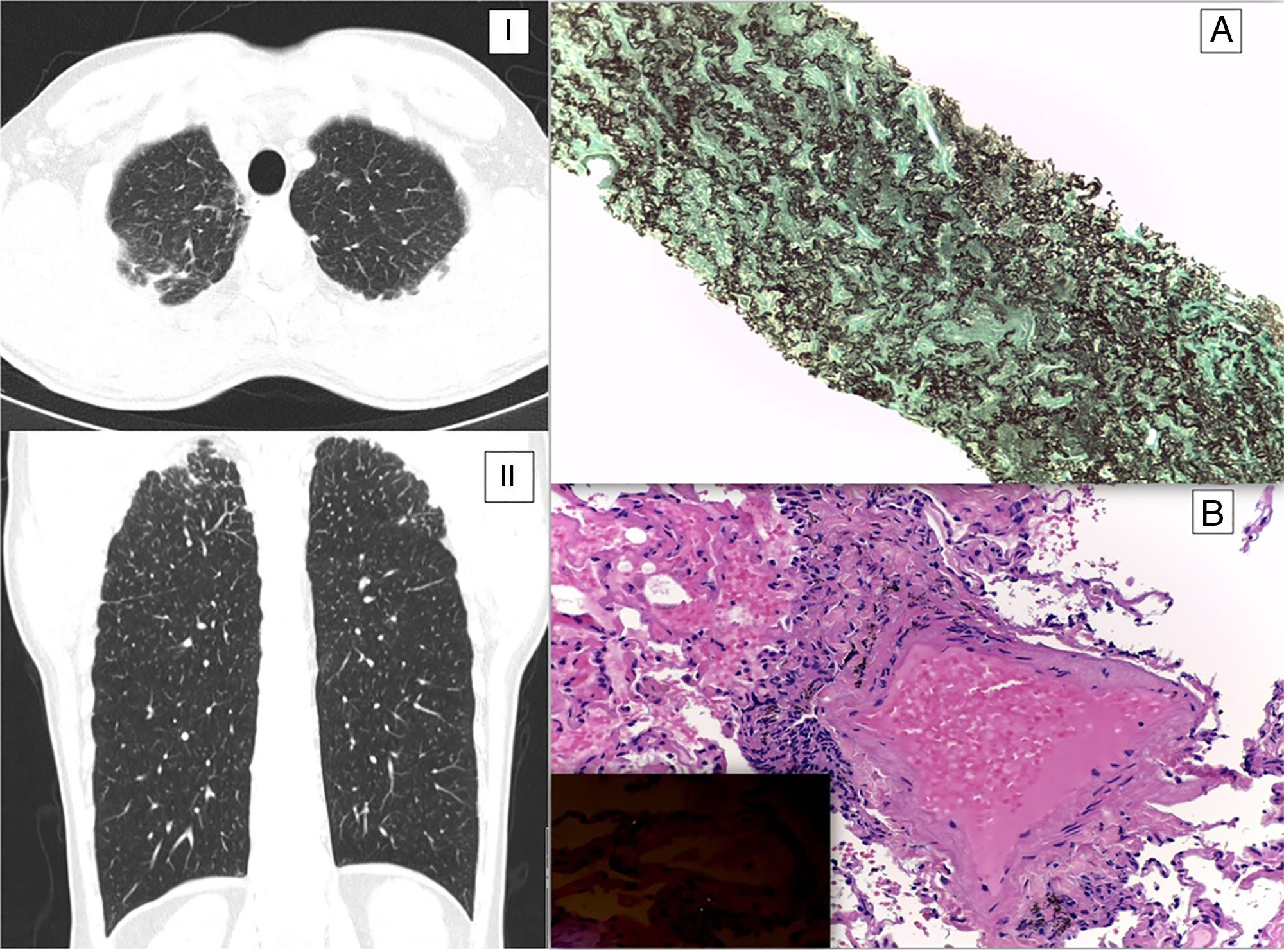
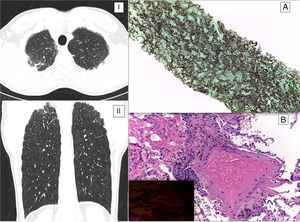
A 47-year-old man, ex-smoker (22 pack-year), working as a plumber in a construction company without any relevant previous medical history before a clinical presentation with dry cough, low-grade fever and weight loss for a month. After an initial primary health care observation, a chest X-ray, which showed fine nodular opacities, was prescribed. The patient was treated with antibiotics with resolution of the symptoms, but the radiological findings did not improve. The high resolution computed tomography (HRCT) of the thorax revealed diffuse micronodular pattern with random distribution, mainly in the upper lobes, apical pleural thickening with extension to the pulmonary parenchyma (Fig. 1 – I and II) and mediastinal and hilar lymphadenopathies. Since radiological features were interpreted as possible mycobacterial lung infection, he was submitted to videobronchofibroscopy with bronchoalveolar lavage for microbiological scrutiny that was negative. Afterwards, a transthoracic core biopsy guided by CT to the apical subpleural lesions was performed and pulmonary parenchyma with fibrosclerosis and extensive septal elastosis (more than 80% of fibroelastic changes in this sample), associated with a discrete lymphoplasmocytic inflammatory infiltrate were reported on histological examination, according with PPFE; no silicate type refractive particles or granulomas were identified (Fig. 1A). The clinical case was then discussed in the diffuse lung diseases multidisciplinary team meeting and although the apical radiological features were consistent with PPFE, the micronodular pattern was not clarified suggesting silicosis/sarcoidosis. Therefore, the patient was submitted to transbronchial lung cryobiopsy that revealed macrophages in peribronchovascular location with anthracotic pigment and the presence of acicular refractive particles in polarized light compatible with silicosis (Fig. 1B).
(I) Axial and coronal (II) HRCT image show pleural and sub pleural thickening with mild fibrotic changes in the marginal parenchyma with apical-caudal distribution. (A) Preservation of the alveolar architecture; marked elastosis in the alveolar septa and obliteration of airspaces by fibrosis (EVG, 100×) – suggestive of pleuropulmonary fibroelastosis. (B) Small aggregates of histiocytes and anthracose pigment around bronchioles (H&E; 200×); birefringent silicate crystals are identified using polarized light (inset) – suggestive of early silico-anthracosis.
The etiology of PPFE is not well established and is considered idiopathic when none of the known associated conditions are identified.5 There are reports of patients with PPFE and dust exposure, but only one has histological confirmation of that exposure (aluminum, silicon and oxygen).6 The present case is the first association with silicosis described, highlighting the eventual relevance of this entity in silica exposure scenario. Occupational exposure to respirable crystalline silica dust particles occurs in many industries. Diagnosis of silicosis needs carefully documented records of occupational exposure and radiological features, with exclusion of other competing diagnoses.7
Concluding, PPFE needs to be considered also in the context of occupational exposure and data are needed regarding the implication of this association in the disease clinical course and prognosis.