Multiple myeloma is the second most common hematological malignancy and usually presents with bone pain, pathologic fractures, and anemia.1 It may affect the thorax as bone lesions, plasmocytomas, pulmonary infiltrations, and pleural effusion.2 Pleural effusion is seen in 6% of the myeloma patients3 but pleural effusion due to plasma cell infiltration is rare, with an incidence of 0.8% and less than 100 cases reported to date.
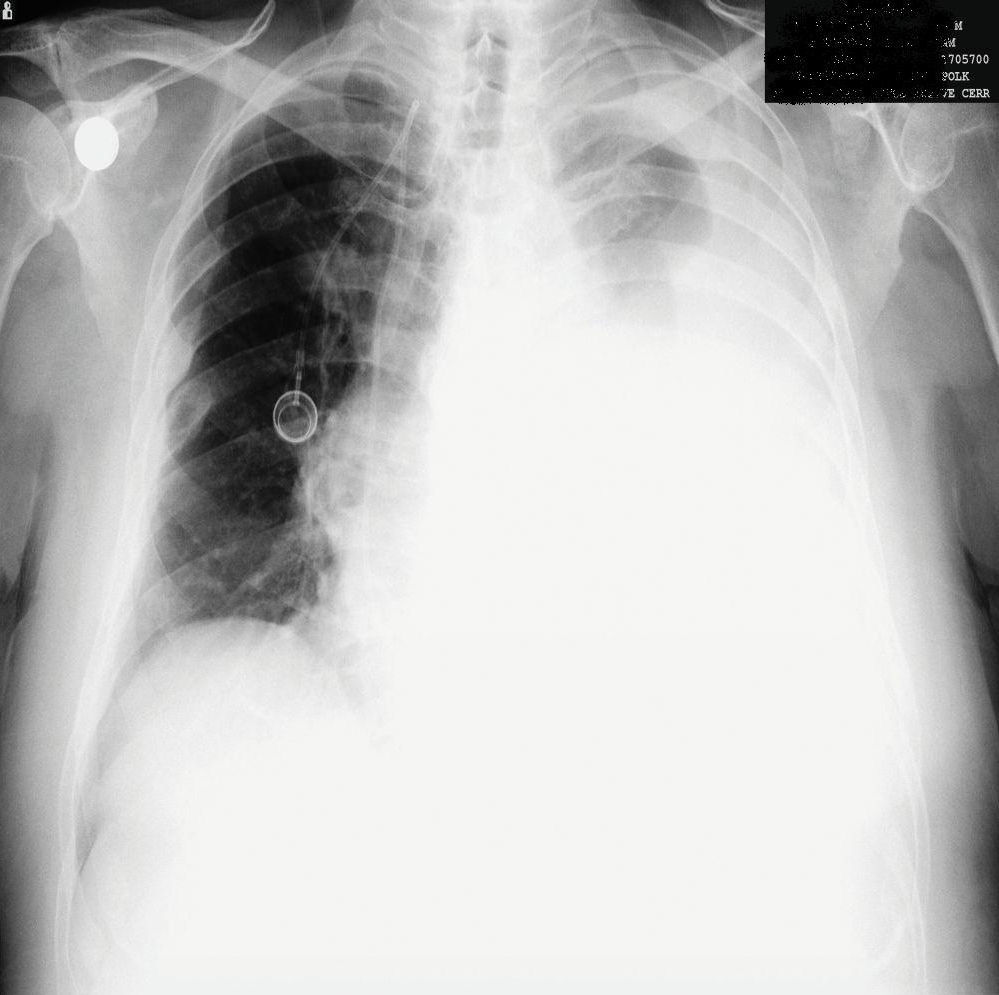
A 62-year-old man was diagnosed with MM (Ig G-kappa), stage IIIA, in June 2010. He was treated with two courses of bortezomib and autologous stem cell transplantation was performed in September 2010. He was given 50mg/day cyclophosphamid as maintenance therapy. In August 2012, he presented with chest pain. A palpable mass in the left hemithorax was detected. X-ray showed multiple rib fractures. PET-CT showed expansive 8×9cm mass located in the left hemithorax in the region of the ninth and tenth ribs (SUV max 15.5). The following were noted in laboratory studies: hemoglobin: 14.1g/dL, white blood cells: 5×109/L, platelets: 242×109/L, creatinine: 0.8mg/dL, uric acid: 6mg/dL, calcium: 10.7mg/dL, total protein: 7.4g/dL, albumin: 4.9g/dL, globulin: 2.5g/dL, kappa: 217mg/dL and β-2 microglobulin: 3668ng/mL. Serum protein electrophoresis was normal, and the 17p13,1 (p53 gene) was negative by FISH. Bone marrow biopsy showed CD138 (+), kappa (+) plasma cell infiltration. The patient was administered lenalidomid–dexamethosone. After two courses, pleural effusion was detected in left hemithorax in November 2012 (Fig. 1). Thoracentesis was performed and revealed exudate with a protein level of 6g/dl. Cytology revealed small lymphocytes, polymorphonuclear leukocytes, mesothelial cells and CD138, IgG and kappa positive atypical plasma cells. HHV-8 was negative in immunohistochemical stain. Bacterial and mycobacterial cultures were negative. Bortezomib treatment was added, but the patient died two months later due to respiratory distress after diagnosis of pleural involvement.
Malignant myelomatous effusion occurs due to infiltration of the pleura by the abnormal proliferation of plasma cells from an extramedullary plasmacytoma of the thoracic wall, lung, or bone. Diagnostic criteria of the myelomatous pleural effusion are: demonstration of a monoclonal protein in pleural fluid electrophoresis, detection of atypical plasma cells in pleural fluid, and histological confirmation by pleural biopsy.4 Pleural cavity involvement has a poor prognosis. Systemic chemotherapy (interferons, bortezomib, thalidomide) radiotherapy, autologous stem cell transplantation, and direct injection of chemotherapeutics into the pleural cavity were administered. There have been only few cases of malignant pleural effusion in which bortezomib was effective, but pleural infiltration is fatal, with a median survival of 1.5–3 months. Thus, more aggressive chemotherapy regimens may be indicated in myeloma with pleural cavity involvement.
AuthorshipDepartment of Hematology +90 232 3903504. Data collection and preparation of manuscript.
Conflict of InterestThe authors declare that they have no conflict of interests.
Please cite this article as: Cömert M, Gürsoy S, Töbü M. Formación de derrame pleural en el curso de un mieloma. Arch Bronconeumol. 2015;51:418–419.