Plastic bronchitis (PB) is a rare, underdiagnosed entity,1–7 characterized by the formation of obstructive bronchial plugs or cylinders of thick, tenacious mucus that cause the collapse of one or more lobes or even a whole lung.1,4–7 These casts are often expectorated, but they might be discovered on bronchoscopy or appear in the bronchial tree during autopsy.4,7 PB is also called fibrinous bronchitis, pseudomembranous bronchitis, or Hoffman's bronchitis.4,6 It has been described in asthma, cystic fibrosis (CF), cyanotic congenital heart diseases, respiratory infections, bronchiectasis, allergic bronchopulmonary aspergillosis (ABPA), acute chest pain in sickle cell disease, alpha thalassemia, etc.1,4–7 The pathogenesis of PB is not well understood.1,4 There are probably 2 mechanisms involved in its development: (1) bronchial injury or changes in bronchial epithelial function due to inflammation or infection, as occurs, for example, in asthma, bronchiectasis, CF, sickle cell anemia, and (2) deterioration of pulmonary lymphatic drainage, as occurs in congenital heart disease.4,6,8 We report a case of PB in a patient with CF, a situation rarely documented in the literature.
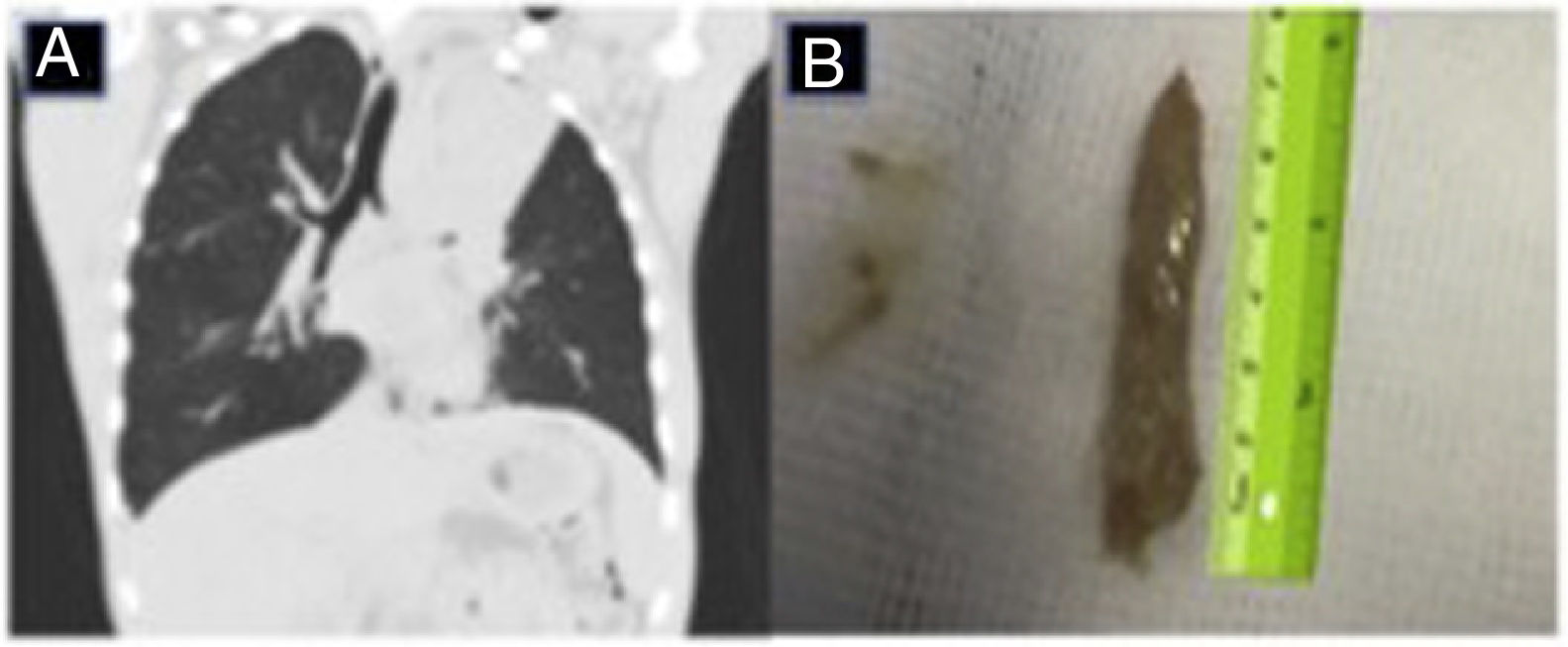
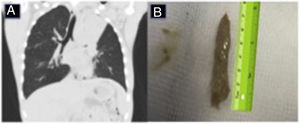
Our patient was a 15-year-old boy with a history of CF, chronically colonized with oxacillin-sensitive Staphylococcus aureus, Haemophilus influenzae, and Pseudomonas aeruginosa, who was admitted for fever of 39°C, asthenia, anorexia, and chest pain in the left hemithorax. Posteroanterior and lateral chest X-ray showed left upper lobe atelectasis. He was admitted for the administration of intravenous antibiotic therapy with piperacillin–tazobactam and tobramycin. The study to rule out other possible causes of atelectasis associated with CF was significant for a total IgE level of 2500IU/ml and Aspergillus fumigatus (AF)-specific IgE of 38.80IU/ml, IgG, precipitins and skin prick positive for AF, so prednisone 60mg every 24h and voriconazole 200mg every 12h were added to the treatment. After 15 days of treatment, clinical but not radiological improvement was observed, so a lung CT was performed that revealed complete atelectasis of the left upper lobe and the presence of a hyperdense cast in the bronchial tree (Fig. 1A). Given these findings, a fiberoptic bronchoscopy (FB) was performed, which revealed an obstruction in the entrance to the bronchus of the left upper lobe, caused by a large mucous plug. Using 4.6mm fiberoptic bronchoscopy with sustained aspiration, a bronchial cast measuring 7×1cm (Fig. 1B) could be extracted, that was diagnosed as PB. One month after extraction of the bronchial cast, clinical and radiological improvement was confirmed, and the tapering and gradual withdrawal of corticosteroids began.
In CF, atelectasis occurs as a result of mucus plugs and severe parenchymal disease.3 It is typically treated with IV antibiotics and intensification of respiratory physiotherapy.3 If clinical and radiological improvement is not achieved, as occurred in our patient, complications such as PB must be considered. Several classifications of PB have been proposed: some are based on the histology of the cast,1,4,9 distinguishing inflammatory PB from non-inflammatory PB, and others on the associated etiology,1 which defines PB as caused by a specific disease, or as idiopathic, if the disease is unknown.1 Madsen et al. recommended a classification based on the associated disease and the histology of the cast, if the etiology of the PB is unclear.1,8 Basic treatment of PB is symptomatic, i.e., improvement of alveolar ventilation and mucociliary clearance, and reduction of inflammation and the bacterial or fungal load1,4,6 in the case of PB caused by bronchial infection or ABPA. Topical treatment of the bronchial cast is not well defined, and no particular mucolytic agent is considered superior to others1; the cast may be difficult to remove with bronchial instillation of physiological saline or bronchoscopic suction.1 Bronchodilators and mucolytics may disintegrate the secretions.1,5 Recombinant human DNase (rhDNase) has been used to reduce the viscoelasticity of sputum in patients with CF.3 In our case, rhDNase was instilled under direct vision bronchoscopy to treat the PB. The use of tissue plasminogen activator (0.7–1mg/kg every 4h) has been described in PB that develops after the Fontan procedure in children.1,4,5,7,10 It has also been reported that inhaled heparin can be effective,7,11 since its anti-inflammatory properties can help reduce mucin secretion, prevent activation of the fibrin tissue factor pathway, and reduce vascular filtration. Inhaled anticholinergics can reduce the formation of casts, and low-dose macrolides can decrease mucin production by inhibiting kinase 1 and 2 activation and reducing the severity of PB.7,12,13 In patients with lymphatic abnormalities, the most effective therapy for PB is selective lymphatic embolization with magnetic resonance-guided lymphography.6,7 The role of FB might be questionable in our patient, but we decided to use this technique, given the failure of conservative medical treatment with IV antibiotics, corticosteroids, and antifungal agents. By using FB, we were able not only to diagnose the PB and instill rhDNase in situ, but we could also extract the bronchial casts, thus improving pulmonary ventilation and mucociliary clearance.
In summary, we hope this report of PB in a patient with CF and ABPA will raise awareness in the community of this diagnostic possibility in patients with CF and persistent atelectasis who fail to improve with standard treatments, such as antibiotics, antifungals, and corticosteroids. Risk factors, such as decreased mucociliary clearance, respiratory tract inflammation or infection, hypereosinophilia, and aspergillosis, must be identified and treated. We defend the early use of FB in patients with CF and persistent atelectasis, to assist in the etiological diagnosis, instillation of mucolytics, and extraction of possible bronchial casts.
Please cite this article as: Delgado Pecellín I, Moreno Ortega M, Carrasco Hernández L, Marín Barrera L, Muñoz Zara P, Moreno Valera MJ, et al. Atelectasia persistente en paciente con fibrosis quística: ¿debemos tratarla siempre con antibioterapia? Arch Bronconeumol. 2019;55:54–55.