Lymphadenopathies in the subaortic and paraaortic stations are difficult to access by fiberoptic bronchoscopy or endobronchial ultrasound, and their cytohistological characterization often requires more invasive (usually surgical) techniques.1–3 Percutaneous biopsy of paraaortic anterior mediastinal lesions is a less invasive technique than surgical exploration of this station. It is useful for obtaining cytological or histological material but complications are not unknown.4 The interposition of important anatomical structures often hinders or prevents a direct percutaneous approach to these lesions.5 Different percutaneous approaches for the anatomopathological diagnosis of anterior mediastinal lesions designed to avoid puncture of the visceral pleura and pulmonary parenchyma have been described in the literature.6 We report the case of a patient with a paraaortic mass that was biopsied percutaneously using a contralateral parasternal approach (CLPA) under radiological guidance following instillation of saline serum into the anterior mediastinal fat (“hydrodissection”).
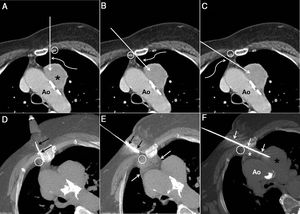
The patient was an obese 74-year-old woman, former smoker (pack-year index=56) with a diagnosis of grade II COPD and moderate sleep apnea-hypopnea syndrome who consulted due to dyspnea and chest pain. A chest X-ray revealed an abnormal mediastinal contour suggestive of tumor disease. A chest computed tomography (CT) confirmed the existence of a solid paraaortic mass in the anterior mediastinum (Fig. 1A) and a small pulmonary nodule in the left upper lobe. Fiberoptic bronchoscopy with bronchial aspiration was initially proposed, but during the procedure the patient developed an episode of oxygen desaturation and hypotension that required discontinuation. Her situation improved following administration of intravenous saline and noninvasive mechanical ventilation. Given the small size of the pulmonary nodule and the patient's poor tolerance of fiberoptic bronchoscopy, we decided to attempt histological sampling of the paraaortic mass by the percutaneous route under radiological guidance. We opted for a parasternal approach to biopsy the mediastinal mass, but left parasternal access would involve puncture of the visceral pleura and the left upper lobe pulmonary parenchyma; moreover, using this approach, the biopsy needle (which has a 1 or 2cm advance mechanism for obtaining histological material) would be aimed directly at the wall of the thoracic aorta, posing a potential risk of injury (Fig. 1A). A CPLA was proposed as an alternative. With this technique, the biopsy needle would be introduced into the chest following the axis of the aortic arch (i.e., parallel to the aortic arch). This contralateral access, whether medial (Fig. 1B) or lateral (Fig. 1C) to the right internal mammary vessels, would also involve puncture of the visceral pleura and pulmonary parenchyma of the right upper lobe. However, taking advantage of the fact that the fat of the anterior mediastinum was in contact with the right parasternal region, two maneuvers were finally selected: (1) to rotate the patient to her right side to shift the anterior mediastinal fat further to that side, allowing the biopsy needle to be inserted through that fat; and (2) to “expand” the anterior mediastinal fat by instilling saline serum (Fig. 1D, “hydrodissection” technique) and, once a “salinoma” had been created in the anterior region of the mediastinum, to safely advance the biopsy needle without puncturing the pleura or pulmonary parenchyma to reach the left paraaortic mass (Fig. 1E and F). The biopsy procedure, performed after obtaining informed consent from the patient, went smoothly; two 18G cylinders were obtained (histological analysis confirmed a small cell carcinoma), and the patient was referred to medical oncology to initiate the appropriate treatment.
(A) Axial CT image of the chest with intravenous contrast medium, showing a paraaortic mass in the anterior mediastinum (asterisk). The straight arrow shows the theoretical path of the biopsy needle in a left parasternal approach between the left inner mammary vessels (circle) and the left edge of the sternum. Note that the aortic arch (Ao) is in the theoretical path of the biopsy needle. The curved arrow shows that the left lung parenchyma would be punctured using this access. (B) Axial CT image of the chest with intravenous contrast medium in which the straight arrow shows the theoretical path of the biopsy needle using a right parasternal medial approach to the right internal mammary vessels (circle). Note that the aortic arch (Ao) is not in the theoretical path of the biopsy needle, but that this approach also punctures the left pulmonary parenchyma (curved arrow). (C) Axial CT image of the chest with intravenous contrast medium in which the straight arrow shows the theoretical path of the biopsy needle using a right parasternal lateral approach to the right internal mammary vessels (circle). Note that the aortic arch (Ao) is also not in the theoretical path of the biopsy needle, but that this approach punctures the right pulmonary parenchyma (curved arrow). (D) Axial CT image of the chest obtained during the biopsy procedure using the CPLA, with the patient in the semi-right lateral decubitus position, showing an intramuscular needle (arrows) between the right internal mammary vessels (circle) and the right sternum margin for local instillation of saline (hydrodissection). (E) Axial CT image of the chest obtained during the biopsy procedure using the CPLA with the patient in the semi-right lateral decubitus position. After expanding the anterior mediastinum using hydrodissection (white arrows), the biopsy needle is inserted (black arrows) into the chest wall. Note that the biopsy needle is directed into the space between the right internal mammary vessels (circle) and the right edge of the sternum. (F) Axial CT image of the chest obtained during the biopsy procedure by CPLA, with the patient in the semi-right lateral decubitus position, where the biopsy needle (arrows) has been advanced to the paraaortic mass (black asterisk) through the space between the right edge of the sternum and the right internal mammary vessels (circle). Note the presence of a “salinoma” (white asterisk) in the anterior mediastinum and the parallel trajectory of the biopsy needle to the aortic arch avoiding any possibility of damaging the aorta (Ao).
Masses and lymphadenopathies in the paraaortic region of the anterior mediastinum are inaccessible by fiberoptic bronchoscopy or endobronchial ultrasound, and anatomopathological typing of these lesions requires more invasive techniques (usually surgery, such as mediastinoscopy or thoracoscopy).1–3 Percutaneous biopsy (CT- or ultrasound-guided) of paraaortic anterior mediastinal lesions is a less invasive technique than surgical exploration and is useful for obtaining cytohistological material, although it is not free from complications (pneumothorax, pulmonary hemorrhage, mediastinal hematoma, phrenic nerve injury, etc.).4 The interposition of important thoracic vessels (internal mammary vessels, aorta and supra-aortic trunks, pulmonary artery trunk), bone and cartilaginous structures (sternum, costal cartilage, clavicles) or the lung itself often make a direct percutaneous approach to anterior mediastinal lesions difficult or impossible.5 Various percutaneous approaches for the pathological diagnosis of anterior mediastinal lesions designed to avoid puncture of the visceral pleura and pulmonary parenchyma have been described in the literature.6 Parasternal access has its own technical particularities and complications, but the major publications in which it is addressed only describe the ipsilateral parasternal approach to the thoracic mass, not the CLPA.4–6 After instilling saline to expand the anterior mediastinum and with the patient placed in a semi-right lateral decubitus position, we were able to advance the biopsy needle painlessly through the fatty tissue of the anterior mediastinum without damaging the internal mammary vessels and without puncturing the parietal pleura or the visceral pleura (or the pulmonary parenchyma). Moreover, advancing the biopsy needle parallel to the aortic arch minimized the risk of injury to the thoracic aorta during needle deployment. Although the injection of saline serum prior to the introduction of the biopsy needle lengthens the procedure by a few minutes, we believe that this is a well-tolerated maneuver that allows safer advancement of the biopsy needle. Some authors have proposed performing echoendoscopic aspirations (through the esophagus) of the paraaortic station through the thoracic aorta, but in our opinion this is a technique that requires a high degree of specialization, sedation, and most importantly, involves risks such as esophageal perforation, mediastinitis, or acute aortic syndrome.7–9 The CPLA for paraaortic lesions does not require patient sedation, can be performed by any radiologist with experience in diagnostic chest interventionism, is relatively painless because it does not require puncture of the pleural surface, and minimizes the risk of vascular injury by advancing the needle parallel to the axis of the aortic arch.
We believe that this percutaneous technique for the biopsy of anterior mediastinal paraaortic lesions using CPLA has not been previously described in the literature. When used alongside hydrodissection and/or positioning of patients in decubitus or semi-lateral decubitus, it offers the possibility of obtaining cytological or histological material safely, relatively painlessly, and without risk of injury to the aortic arch.
Please cite this article as: Gorospe L, Ayala-Carbonero AM, Montelongo-Martín A, Mirambeaux-Villalona RM, Arrieta P, Muñoz-Molina GM, et al. Biopsia percutánea de masa mediastínica paraaórtica mediante abordaje paraesternal contralateral: un nuevo acceso alternativo seguro. Arch Bronconeumol. 2021;57:499–501.